ABSTRACT
Objective: To estimate the prevalence of undiagnosed COPD among individuals with risk factors for the disease treated at primary health care clinics (PHCCs) in the city of Aparecida de Goiânia, Brazil. Methods: Inclusion criteria were being ≥ 40 years of age, having a > 20 pack-year history of smoking or a > 80 hour-year history of exposure to biomass smoke, and seeking medical attention at one of the selected PHCCs. All subjects included in the study underwent spirometry for the diagnosis of COPD. Results: We successfully evaluated 200 individuals, mostly males. The mean age was 65.9 ± 10.5 years. The diagnosis of COPD was confirmed in 63 individuals, only 18 of whom had been previously diagnosed with COPD (underdiagnosis rate, 71.4%). There were no significant differences between the subgroups with and without a previous diagnosis of COPD in relation to demographics and risk factors. However, there were significant differences between these subgroups for the presence of expectoration, wheezing, and dyspnea (p = 0.047; p = 0.005; and p = 0.047, respectively). The FEV1 and FEV1/FVC ratio, expressed as percentages of the predicted values, were significantly lower in the subjects with a previous diagnosis of COPD, which was predominantly mild or moderate in both subgroups. Conclusions: The rate of underdiagnosis of COPD was high at the PHCCs studied. One third of the patients with risk factors for COPD met the clinical and functional criteria for the disease. It seems that spirometry is underutilized at such facilities.
Keywords:
Pulmonary disease, chronic obstructive/diagnosis; Primary health care; Spirometry.
RESUMO
Objetivo: Estimar a prevalência de DPOC não diagnosticada entre indivíduos com fatores de risco para a doença atendidos em unidades de estratégia de saúde da família (UESF) na cidade de Aparecida de Goiânia (GO). Métodos: Os critérios de inclusão foram ter idade ≥ 40 anos, ter história de tabagismo > 20 maços-ano ou de exposição à queima de biomassa > 80 horas-ano e procurar atendimento médico em uma das UESF selecionadas. Todos os indivíduos incluídos no estudo foram submetidos a espirometria para a definição diagnóstica de DPOC. Resultados: Foram avaliados com sucesso 200 indivíduos, a maioria do sexo masculino. A média de idade foi de 65,9 ± 10,5 anos. Tiveram confirmação diagnóstica de DPOC 63 indivíduos. Desses, apenas 18 haviam sido previamente diagnosticados com DPOC (taxa de subdiagnóstico de 71,4%). Não houve diferenças significantes entre os subgrupos com e sem diagnóstico prévio de DPOC em relação a fatores demográficos e fatores de risco. Entretanto, houve diferenças significantes entre esses subgrupos em relação à presença de expectoração, chiado e dispneia (p = 0,047, p = 0,005 e p = 0,047, respectivamente). Os valores de VEF1 e VEF1/CVF, em percentual do previsto, foram significativamente menores nos indivíduos com diagnóstico prévio de DPOC. A DPOC foi predominantemente leve a moderada em ambos os subgrupos. Conclusões: A taxa de subdiagnóstico da DPOC foi alta nas UBS estudadas. Um terço dos pacientes com fatores de risco para DPOC apresentou critérios clínicos e funcionais para a doença. A espirometria foi subutilizada.
Palavras-chave:
Doença pulmonar obstrutiva crônica/diagnóstico; Atenção primária à saúde; Espirometria.
IntroductionChronic respiratory diseases represent a major public health problem worldwide, affecting quality of life, leading to physical disability, and having a major socioeconomic impact.(1)
The mortality from COPD is expected to increase by 30% over the next 10 years unless measures are taken in order to reduce the risk factors for COPD and the underdiagnosis of the disease. It has been estimated that, by 2030, COPD will have become the third leading cause of death worldwide.(1)
In the worldwide fight against COPD, underdiagnosis and the consequent lack of treatment are the primary targets. Another important facet of COPD is that it is not seen as a systemic disease and therefore is not evaluated by the system for the surveillance of chronic diseases, including cardiovascular and metabolic diseases.(1)
Studies and interventions focusing on the diagnosis of COPD at primary health care clinics (PHCCs) are needed in order to detect the disease in a timely manner and control it more effectively. The objective of the present study was to screen for COPD in patients being treated at PHCCs and having risk factors for the disease but not routinely screened for COPD at such clinics.
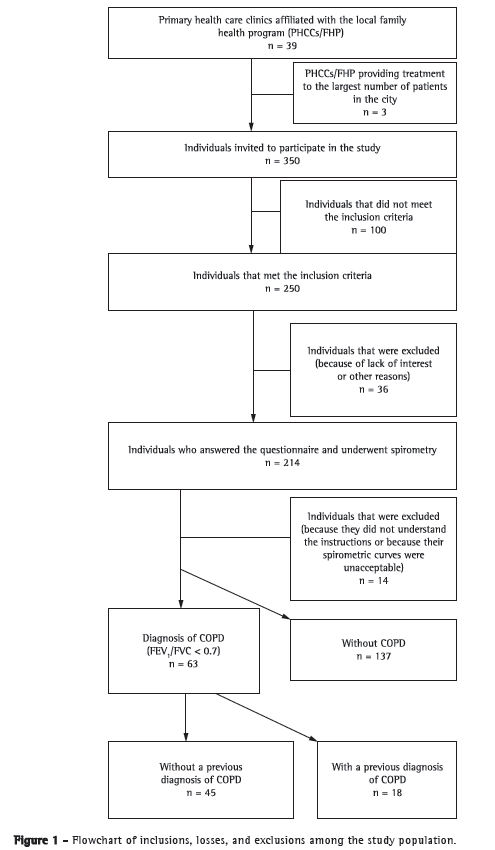
MethodsThis was an analytical, observational, cross-sectional study conducted between May and September of 2011 at three PHCCs affiliated with the Family Health Program in the city of Aparecida de Goiânia, Brazil. The city is located in the metropolitan area of Goiânia and has an estimated population of 500,000 inhabitants. The study received support from the managers of the Aparecida de Goiânia Municipal Department of Health. The selected PHCCs were chosen from among those providing treatment to the largest number of patients (in the southern, eastern, and western regions of the city). These PHCCs provide treatment to 27% of all patients being treated at PHCCs in the city of Aparecida de Goiânia (according to information from the municipal department of health). Individuals seeking the selected PHCCs for routine outpatient treatment and having no acute respiratory symptoms were invited to answer questions regarding demographics and risk factors for COPD. Inclusion criteria were being 40 years of age, having a 20 pack-year history of smoking or a 80 hour-year history of exposure to biomass smoke (or both), and having given written informed consent. We excluded individuals with a previous diagnosis of bronchial asthma, allergic rhinitis, chronic lung diseases other than COPD, or extrapulmonary disease potentially affecting lung function, as well as those who did not meet the criteria for spirometry (Figure 1).
The individuals who met the inclusion criteria answered a modified version of the principal questionnaire used in a prevalence study.(2) We collected demographic and clinical data (respiratory symptoms, such as cough, expectoration, wheezing, and dyspnea, as well as a previous diagnosis of emphysema, chronic bronchitis, or COPD, with or without spirometry), as well as variables related to exposure to tobacco smoke and smoke from wood-burning stoves.
The quantification of exposure to smoke from wood-burning stoves was based on the exposure levels considered significant in previous studies.(2)
For the assessment of lung function, we used a Spirotrac® spirometer (Vitalograph, Buckingham, UK), which was calibrated daily. Spirometry was performed before and after bronchodilator use, in accordance with the Brazilian Thoracic Association criteria,(3) and the results were interpreted in accordance with the values predicted by Pereira et al.(4) We studied the following spirometric variables: FVC; FEV1; and FEV1/FVC.
The diagnosis of COPD was based on a post-bronchodilator FEV1/FVC < 0.70 (in absolute values). In order to determine the severity of COPD, we used the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria.(1)
Patients with a presumptive diagnosis of COPD were defined as those who had previously been diagnosed with emphysema, chronic bronchitis, or COPD.
We calculated the sample size by estimating the proportion of the population with specific absolute accuracy and by using a formula.(5) We assumed the maximum prevalence of COPD in the city population to be 25%, on the basis of the results of a study of the prevalence of COPD in five Latin American cities.(2) With a confidence level of 95% and an absolute accuracy of 6%, the minimum sample size was determined to be 200 individuals.
For statistical analysis, we used the Statistical Package for the Social Sciences, version 15 (SPSS Inc., Chicago, IL, USA), logistic regression analysis being performed and ORs being calculated. The level of statistical significance was set at p < 0.05.
The present study was approved by the Human Research Ethics Committee of the Federal University of Goiás Hospital das Clínicas (Protocol no. 202/2010).
ResultsWe selected 200 individuals, 63 of whom were diagnosed with COPD. The mean age of the participants was 65.0 ± 10.40 years, individuals in the 60-80 year age bracket having predominated. Most of the participants had a low level of education, and most identified themselves as Mulattos.
Regarding risk factors (smoking history, exposure to smoke from wood-burning stoves, and type of cigarette smoked), there were no statistically significant differences between the individuals with COPD and those without.
Of the 63 individuals diagnosed with COPD, 45 reported no previous diagnosis of COPD, the rate of underdiagnosis being therefore 71.4%. Of the 137 individuals who did not meet the diagnostic criteria for COPD, 20 reported a previous diagnosis of COPD, the rate of misdiagnosis or overdiagnosis being therefore 14.6%.
Only 5.6% of the individuals with a previous diagnosis of COPD had undergone spirometry. The 200 individuals under study had risk factors that constituted an indication for spirometry (i.e., smoking and exposure to smoke from wood-burning stoves), and the rate of use of spirometry as a diagnostic tool was 1.5%.
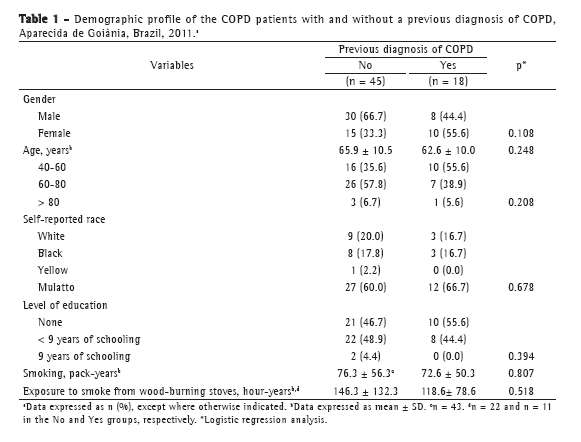
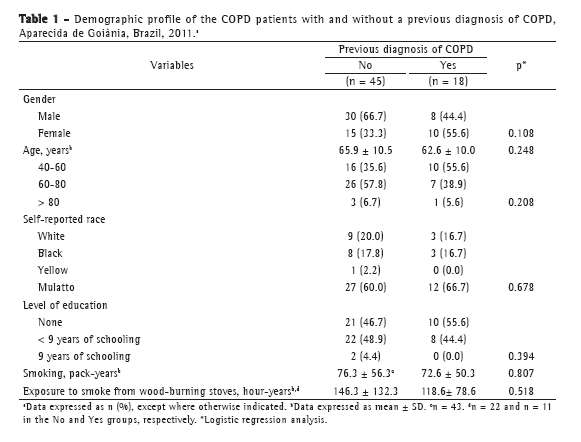
There were no statistically significant differences between the groups with and without a previous diagnosis of COPD in terms of gender, age, race, or level of education. In addition, there were no statistically significant differences between the groups in terms of smoking history or cumulative exposure to smoke from wood-burning stoves. In the group of COPD patients without a previous diagnosis of COPD, the mean age was 65.9 ± 10.5 years, and there was a predominance of the following: males; self-reported Mulattos; and a low level of education (< 9 years of schooling). In addition, the mean smoking history was 76.3 ± 56.3 pack-years, and the mean cumulative exposure to smoke from wood-burning stoves was 146.0 ± 132.3 hour-years (Table 1).
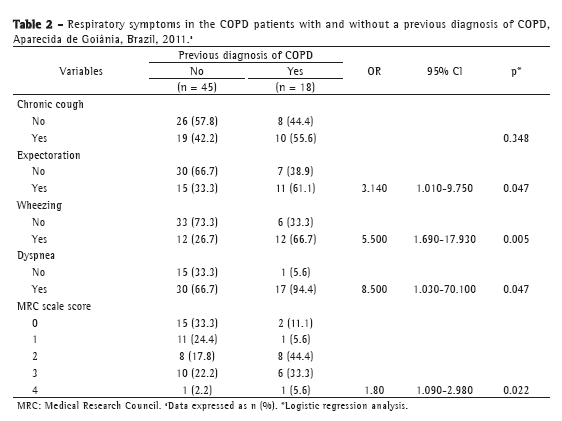
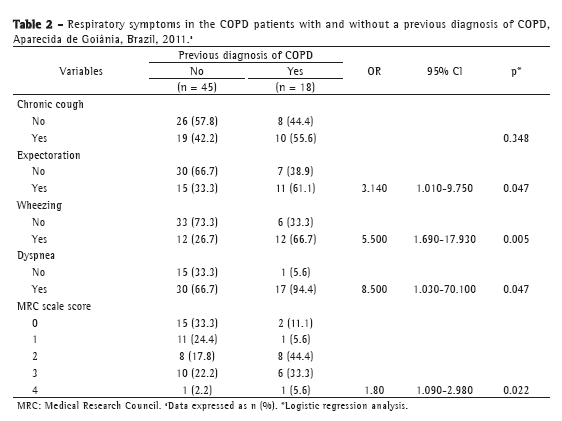
Cough, expectoration, wheezing, and dyspnea were more common in the COPD patients with a previous diagnosis of COPD than in those without, the two groups of patients being significantly different only in terms of expectoration, wheezing, and dyspnea. The degree of dyspnea in 44.4% of the patients with a previous diagnosis of COPD was 2, as assessed by the Medical Research Council scale (Table 2).
The FEV1 and FEV1/FVC ratio, expressed as percentages of the predicted values, were significantly lower in the individuals with a previous diagnosis of COPD. As can be seen in Table 3, COPD was predominantly mild or moderate in the group of patients without a previous diagnosis of COPD.
 Discussion
DiscussionThe rate of underdiagnosis of COPD in individuals having risk factors for the disease and being treated at PHCCs was found to be 71.4% in the present study. In the individuals with a previous diagnosis of COPD, the clinical expression of the disease was more severe and the degree of bronchial obstruction was higher.
The authors of a study aimed at documenting the extent of underdiagnosis of COPD in at-risk patients treated at PHCCs suggested that 10-20% of undiagnosed COPD cases can be detected if smokers over 40 years of age are screened.(6) They also drew attention to the probable reasons for the underdiagnosis of COPD, stating that physicians are not fully aware of the importance of risk factors for and symptoms of COPD, and that they lack knowledge of the spirometric criteria for the disease. In addition, the authors stated that patients seek medical attention only when the symptoms affect their quality of life.
In the present study, we found no differences between the subgroups of patients with and without a previous diagnosis of COPD in terms of risk factors (smoking and cumulative exposure to smoke from wood-burning stoves) or demographics.
In the present study, the mean age of the patients with COPD was higher than was that of those without. Age is often reported as a risk factor for COPD.(1,2) Several studies have shown that the proportion of COPD cases tends to increase with age.(7-9)
Data from different studies published in various parts of the world confirm that COPD is underdiagnosed (especially in females) and that the disease is more frequently diagnosed in males than in females (especially among patients being treated at PHCCs).(10,11)
In addition to smoking, exposure to biomass smoke is a risk factor for COPD in developing countries (such as Brazil), principally in rural areas, where women cook in poorly ventilated environments. In a study conducted in Brazil,(12) COPD was diagnosed in 47 of 160 females selected from among those being treated at PHCCs and showing a cumulative exposure to smoke from wood-burning stoves of 211.2 ± 98.2 hour-years.
Jain et al.(13) evaluated 702 COPD patients in terms of etiologic and risk factors for the disease, as well as investigating differences between the genders in terms of clinical presentation, radiological presentation, and comorbidities. The authors found that, in addition to being younger and having reported more symptoms and exacerbations, females showed a higher prevalence of systemic features. Exposure to tobacco smoke predominated among males, whereas exposure to biomass smoke predominated among females. The authors emphasized that an understanding of these differences aids in establishing an early diagnosis of COPD in females.
In the present study, the level of education was found to be lower in the individuals with COPD than in those without, a finding that is consistent with those of studies examining the relationship between COPD and smoking and between COPD and cumulative exposure to biomass smoke.(1,2,14) Those studies showed that a low socioeconomic status and a low level of education are risk factors for COPD, and that the prevalence of COPD tends to decrease as the level of education increases.
Hamers et al.(15) conducted a study in northern and northeastern Brazil in order to determine the prevalence of chronic respiratory diseases in patients treated at PHCCs. The authors emphasized that most of the general practitioners had been trained within specialist settings and were unaware of the prevalence of COPD in the population. A bivariate analysis showed that advanced age, male gender, smoking, and presence of two respiratory symptoms were strong predictors of COPD in the initial evaluation of patients treated at PHCCs.
In the present study, the prevalence of symptoms was higher in the COPD patients with a previous diagnosis of COPD than in those without, suggesting that patients with more symptoms are more easily diagnosed. This is worrisome because it suggests that the diagnosis of COPD was made in the advanced stages of the disease, in which the clinical expression of the disease is more severe. This hypothesis has been raised in another study.(16)
In the present study, the presence of dyspnea in isolation was more common in the individuals with a previous diagnosis of COPD (including those who had been misdiagnosed as having COPD), suggesting that the symptom of dyspnea had been erroneously correlated with pulmonary emphysema and, consequently, COPD. The individuals with a previous diagnosis of COPD had a higher degree of obstruction, as evidenced by the FEV1 values in percentage of predicted. This might be due to the fact that respiratory symptoms are more common in the more advanced stages of the disease. Guidelines provided by the GOLD(1) underscore the role of programs for early detection of COPD and recommend that all available data be used in order to diagnose COPD when spirometry is not available.
Hill et al.(17) found that approximately one in every five adults having risk factors for COPD and seeking a PHCC (for any reason) met spirometric criteria for COPD. Although more than three quarters of the patients with COPD reported at least one respiratory symptom, two thirds were unaware of their diagnosis. The authors concluded that selecting individuals for spirometry on the basis of symptoms alone will identify less than half of the patients with moderate to severe COPD, and that spirometric data should complement the data obtained by surveillance questionnaires. Other studies have suggested that adults seeking treatment at PHCCs and presenting with risk factors for COPD and typical respiratory symptoms should be priority targets for screening and early intervention.(18-20)
In the present study, the COPD patients with a previous diagnosis of COPD had a higher degree of obstruction, as evidenced by the FEV1 values in percentage of predicted. This might have been due to the fact that respiratory symptoms were more common in that subgroup. In both groups, mild to moderate obstruction predominated, a finding that is consistent with those of other studies.(18,21)
In addition to an underdiagnosis rate of 71.4%, we found an overdiagnosis rate of 14.6% and a rate of use of spirometry as a diagnostic tool of 1.5%. These findings are consistent with those of other studies,(2,14,22) in which the rate of use of spirometry to diagnose COPD at PHCCs was found to be low.
The method used in the present study does not allow us to extrapolate our results to a larger population. This might have been possible had we used the methodology commonly used in prevalence studies. However, our study was conducted at PHCCs (where physicians are general practitioners), i.e., clinics that are representative of the primary health care system in the state of Goiás.
Given the high rate of underdiagnosis of COPD in individuals having risk factors for the disease and being treated at PHCCs, we believe that active surveillance for COPD and spirometry are measures that can play a major role in controlling the disease.
References1. Global Initiative for Chronic Obstructive Lung Disease - GOLD [homepage on the Internet]. Bethesda: Global Initiative for Chronic Obstructive Lung Disease [cited 2011 Dec 26]. Global Strategy for the Diagnosis, Management, and Prevention of COPD - Revised 2011. [Adobe Acrobat document, 90p.]. Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2011_Feb21.pdf
2. Menezes AM, Perez-Padilla R, Jardim JR, Muiño A, Lopez MV, Valdivia G, et al. Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366(9500):1875-81. http://dx.doi.org/10.1016/S0140-6736(05)67632-5
3. Sociedade Brasileira de Pneumologia e Tisiologia. Diretrizes para testes de função pulmonar. J Pneumol. 2002;28(Suppl 3):S2-S238.
4. Pereira CA, Sato T, Rodrigues SC. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007;33(4):397-406. PMid:17982531. http://dx.doi.org/10.1590/S1806-37132007000400008
5. Lwanga SK, Lemeshow S. Sample Size Determination in Health Studies. Geneva: World Health Organization; 1991.
6. Tinkelman DG, Price D, Nordyke RJ, Halbert RJ. COPD screening
efforts in primary care: what is the yield? Prim Care Respir J. 2007;16(1):41-8. PMid:17297526. http://dx.doi.org/10.3132/pcrj.2007.00009
7. Yamasaki A, Hashimoto K, Hasegawa Y, Okazaki R, Yamamura M, Harada T, et al. COPD is frequent in conditions of comorbidity in patients treated with various diseases in a university hospital. Int J Chron Obstruct Pulmon Dis. 2010;5:351-5. PMid:21037959 PMCid:2962301. http://dx.doi.org/10.2147/COPD.S12669
8. Lundbäck B, Gulsvik A, Albers M, Bakke P, Rönmark E, van den Boom G, et al. Epidemiological aspects and early detection of chronic obstructive airway diseases in the elderly. Eur Respir J Suppl. 2003;40:3s-9s. PMid:12762567. http://dx.doi.org/10.1183/09031936.03.00403103
9. Lindberg A, Jonsson AC, Rönmark E, Lundgren R, Larsson LG, Lundbäck B. Prevalence of chronic obstructive pulmonary disease according to BTS, ERS, GOLD and ATS criteria in relation to doctor's diagnosis, symptoms, age, gender, and smoking habits. Respiration. 2005;72(5):471-9. PMid:16210885. http://dx.doi.org/10.1159/000087670
10. de Torres Tajes JP, Macario CC. Chronic obstructive pulmonary disease in women [Article in Spanish]. Arch Bronconeumol. 2010;46 Suppl 3:23-7. http://dx.doi.org/10.1016/S0300-2896(10)70023-5
11. Soares S, Costa I, Neves AL, Couto L. Caracterização de uma população com risco acrescido de DPOC. Rev Port Pneumol. 2010;16(2):237-52. Pmid:20437002.
12. Moreira MA. Avaliação de aspectos pulmonares em mulheres expostas à fumaça de combustão de lenha [thesis]. Goiânia: Universidade federal de Goiás; 2011.
13. Jain NK, Thakkar MS, Jain N, Rohan KA, Sharma M. Chronic obstructive pulmonary disease: Does gender really matter? Lung India. 2011;28(4):258 62. PMid:22084538 PMCid:3213711. http://dx.doi.org/10.4103/0970-2113.85686
14. Peña VS, Miravitlles M, Gabriel R, Jiménez-Ruiz CA, Villasante C, Masa JF, et al. Geographic variations in prevalence and underdiagnosis of COPD: results of the IBERPOC multicentre epidemiological study. Chest. 2000;118(4):981-9. PMid:11035667. http://dx.doi.org/10.1378/chest.118.4.981
15. Hamers R, Bontemps S, van den Akker M, Souza R, Penaforte J, Chavannes N. Chronic obstructive pulmonary disease in Brazilian primary care: Diagnostic competence and case-finding. Prim Care Respir J. 2006;15(5):299 306. PMid:16978923. http://dx.doi.org/10.1016/j.pcrj.2006.07.008
16. Llauger Roselló MA, Pou MA, Domínguez L, Freixas M, Valverde P, Valero C, et al. Treating COPD in chronic patients in a primary-care setting [Article in Spanish]. Arch Bronconeumol. 2011;47(11):561-70. PMid:22036593. http://dx.doi.org/10.1016/j.arbres.2011.10.001
17. Hill K, Goldstein RS, Guyatt GH, Blouin M, Tan WC, Davis LL, et al. Prevalence and underdiagnosis of chronic obstructive pulmonary disease among patients at risk in primary care. CMAJ. 2010;182(7):673-8. PMid:20371646 PMCid:2855915. http://dx.doi.org/10.1503/cmaj.091784
18. Geijer RM, Sachs AP, Hoes AW, Salomé PL, Lammers JW, Verheij TJ. Prevalence of undetected persistent airflow obstruction in male smokers 40-65 years old. Fam Pract. 2005;22(5):485-9. PMid:15964866. http://dx.doi.org/10.1093/fampra/cmi049
19. McIvor RA, Tashkin DP. Underdiagnosis of chronic obstructive pulmonary disease: a rationale for spirometry as a screening tool. Can Respir J. 2001;8(3):153-8. Pmid:11420591.
20. Hill K, Hodder R, Blouin M, Heels-Ansdell D, Guyatt G, Goldstein R. Identifying adults at risk of COPD who need confirmatory spirometry in primary care: Do symptom-based questions help? Can Fam Physician. 2011;57(2):e51-7. PMid:21642706 PMCid:3038833.
21. Siatkowska H, Kozielski J, Ziora D. Patients with chronic obstructive pulmonary disease in the primary care setting. Pneumonol Alergol Pol. 2010;78(2):112-20. Pmid:20306422.
22. Chapman KR, Tashkin DP, Pye DJ. Gender bias in the diagnosis of COPD. Chest. 2001;119(6):1691-5. PMid:11399692. http://dx.doi.org/10.1378/chest.119.6.1691
* Study carried out at the Federal University of Goiás, Goiânia, Brazil.
Correspondence to: Maria Conceição C. A. M. de Queiroz. Serviço de Pneumologia, Hospital das Clínicas da UFG, Primeira Avenida, s/n, 2º andar, Setor Leste Universitário, CEP 746005-020, Goiânia, GO, Brasil.
Tel. 55 62 3093-4744. E-mail: sissibb@ig.com.br
Financial support: This study received financial support from the Fundação de Amparo à Pesquisa do Estado de Goiás (FAPEG, Goiás Research Foundation).
Submitted: 3 July 2012. Accepted, after review: 14 September 2012.
About the authors Maria Conceição de Castro Antonelli Monteiro de Queiroz
Attending Physician. Pulmonology Department. Federal University of Goiás School of Medicine Hospital das Clínicas, Goiânia, Brazil.
Maria Auxiliadora Carmo Moreira
Associate Professor. Federal University of Goiás School of Medicine, Goiânia, Brazil.
Marcelo Fouad Rabahi
Adjunct Professor. Federal University of Goiás School of Medicine, Goiânia, Brazil.