ABSTRACT
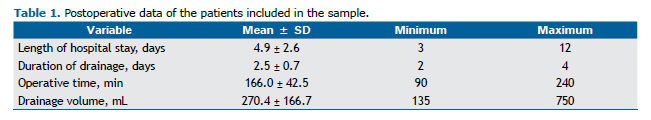
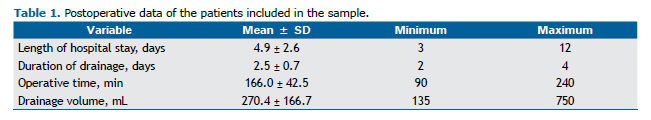
Objective: To report an initial experience with a digital drainage system during the postoperative period of pediatric thoracic surgery. Methods: This was a prospective observational study involving consecutive patients, ≤ 14 years of age, treated at a pediatric thoracic surgery outpatient clinic, for whom pulmonary resection (lobectomy or segmentectomy via muscle-sparing thoracotomy) was indicated. The parameters evaluated were air leak (as quantified with the digital system), biosafety, duration of drainage, length of hospital stay, and complications. The digital system was used in 11 children (mean age, 5.9 ± 3.3 years). The mean length of hospital stay was 4.9 ± 2.6 days, the mean duration of drainage was 2.5 ± 0.7 days, and the mean drainage volume was 270.4 ± 166.7 mL. The mean maximum air leak flow was 92.78 ± 95.83 mL/min (range, 18-338 mL/min). Two patients developed postoperative complications (atelectasis and pneumonia, respectively). The use of this digital system facilitated the decision-making process during the postoperative period, reducing the risk of errors in the interpretation and management of air leaks.
Keywords:
Drainage; Thoracic surgery; Pediatrics.
RESUMO
Objetivo: Relatar a experiência inicial com um sistema de drenagem digital no pós-operatório de cirurgia torácica pediátrica. Métodos: Estudo observacional e prospectivo envolvendo pacientes consecutivos do ambulatório de cirurgia torácica pediátrica da instituição, com idade até 14 anos, e com indicação de ressecção pulmonar (lobectomia e/ou segmentectomia através de toracotomia poupadora muscular). Os parâmetros avaliados foram perda aérea (quantificada com o sistema digital), biossegurança, tempo de drenagem, tempo de internação e complicações. Resultados: O sistema digital foi utilizado em 11 crianças, com média de idade de 5,9 ± 3,3 anos. A média do tempo de internação foi de 4,9 ± 2,6 dias, a de tempo de drenagem foi de 2,5 ± 0,7 dias, e a de volume de drenagem foi de 270,4 ± 166,7 ml. A média da perda aérea máxima foi de 92,78 ± 95,83 ml/min (variação, 18-338 ml/min). Dois pacientes apresentaram complicações pós-operatórias (atelectasia e pneumonia, respectivamente). Conclusões: O uso desse sistema digital facilitou a tomada de decisão durante o pós-operatório, diminuindo o risco de erros na interpretação e no manejo da perda aérea.
Palavras-chave:
Drenagem; Cirurgia torácica; Pediatria.
INTRODUCTIONMost patients undergoing lung surgery require adequate drainage of the pleural cavity to remove air or fluid and to allow expansion of the remaining lung. It is necessary that the health care team be qualified to manage the drainage system correctly.(1) The measurement or grading of air leaks is still subjective and depends on the level of experi-ence of professionals in quantifying them. Therefore, the interpretation of air leaks is related to observer variabil-ity.(1,2) Interobserver disagreement may occur, even between experienced observers. When uncertainty resulting from the use of a traditional system persists, the chest tube may be closed and radiographic assessment may be performed. In such cases, the patient remains in the hospital for at least another day, which results in greater use of resources and time.
In recent years, clinical signs, such as blood pressure, HR, SpO2, and temperature, have been recorded continuous-ly and digitally. Electronic health records and health information technology reduce medical errors because they ensure complete information about the patient's condition.(3) However, to date, air leak information has been ob-tained subjectively. There is also uncertainty about the amount of fluid. Recent studies on digital drainage systems have presented an objective evaluation of these parameters, but, until now, no such studies have been conducted in children. The objective of the present study was to report our initial experience with a digital drainage system during the postoperative period of pediatric thoracic surgery.
METHODSThis was a prospective, consecutive, observational case-series study performed to evaluate the use of a digital drainage system during the postoperative period of pediatric thoracic surgery. This study is part of a project called Dreno Digital and was approved by the Research Ethics Committee of the Federal University of São Paulo/plataforma Brasil (Ruling no. 56579/2012; CAAE: 03514312.1.0000.5505).
The inclusion criteria were as follows: being treated at a pediatric thoracic surgery outpatient clinic; being ≤ 14 years of age; and having an indication for pulmonary resection (lobectomy or segmentectomy via muscle-sparing thoracotomy). The exclusion criteria were as follows: renal or hepatic failure; neurological dysfunction; reoperation; emergency operation; preoperative chemotherapy or radiotherapy; and chest wall resection.
The digital drainage system used was a Thopaz® device (Medela AG, Baar, Switzerland). The parameters evaluated were air leak, biosafety, duration of drainage, length of hospital stay, and complications. In children, there are no established data or parameters regarding when the chest tube can be removed; therefore, we defined an air leak flow < 10 mL/min in the last 6 h as the threshold for removal.
RESULTSThe digital drainage system was used in 11 children in this initial phase. Of those, 4 (36%) were male and 7 (64%) were female. The mean age was 5.9 ± 3.3 years (range, 1.6-13.0 years), with a median of 5 years. The remaining sample data are given in Table 1.
The most common clinical condition was recurrent infection, in 8 patients (72.7%). Pulmonary malformation was the most common diagnosis, in 6 patients (54.5%). Of those 6 patients, 2 had pulmonary sequestration and 4 had cystic adenomatoid malformation. Bronchiectasis was present in 5 patients (45.5%). The procedures performed included pulmonary lobectomy, in 7 patients (63.6%); segmentectomy, in 2 (18.2%); and lobectomy plus segmentectomy, in 2 (18.2%).
Only one chest tube was placed in each patient. The complication rate was 18%, complications occurring in 2 of the 11 patients (atelectasis and pneumonia, respectively). There was no mortality.
Simple tracheal intubation was performed in 10 (91%) of the patients. Only 1 patient underwent selective intuba-tion. All patients were extubated in the operating room, and 7 (64%) stayed in the ICU in the immediate postopera-tive period.
In-hospital analgesia was provided via an epidural catheter in 8 (72.7%) of the patients, all 8 of whom received a solution of 0.25% bupivacaine and fentanyl (mean, 27.7 ± 16.9 mL; range, 5-55 mL). The mean amount of intrave-nous or oral dipyrone was 8.4 ± 4.8 g (range, 2.5-18.0 g), whereas the mean amount of intravenous or oral tramadol was 118.3 ± 154.43 mg (range, 0-550 mg). All children underwent pulmonary resection via intercostal nerve-sparing thoracotomy using the intercostal muscle flap technique. None of the patients had rib fractures or required blood transfusion during the postoperative period. The mean intraoperative blood loss was 45.5 ± 35.3 mL (range, 10-100 mL). Cefuroxime was used for antibiotic prophylaxis
None of the patients had subcutaneous emphysema. Routine suction was performed until postoperative day 1 and was continued thereafter if there was no adequate lung expansion, as confirmed by chest X-ray. Only 1 patient re-quired continuous suction until postoperative day 2. Air leak management efficiency was increased because there was no uncertainty about bubbling, regardless of the rater. Air leak flow was quantified objectively, in mL/min, the mean maximum being 92.78 ± 95.83 mL/min (range, 18-338 mL/min) and the median being 89 mL/min. All chest tubes were removed when the air leak flow was < 10 mL/min: 0 mL/min and 1 mL/min, respectively, in 10 patients and 1 patient. None of the patients required further drainage or had a > 4-cm residual pleural cavity.
The information provided by the device was exported to a computer using the ThopEasy® software (Medela AG). We thus obtained more parameters, such as duration of drainage, date, start time, end time, maximum suction pressure, minimum suction pressure, maximum air leak flow, and minimum air leak flow. The data were displayed in chart and graph formats (Figure 1).
 DISCUSSION
DISCUSSIONBiosafety refers to interventions focused on risk protection, prevention, and minimization for health care profes-sionals and patients. It consists of measures adopted to prevent activity-related risks and involves the relationships among technology, risks, the human factor, and the environment. In this study, biosafety measurement was subjec-tive, and biosafety was favorably assessed by the nursing staff because of the optimization of patient care time. The management process of the digital system was improved as compared with that of a traditional system, given that there was no need for replacing the water seal daily, caring for the bottle, clamping the system, providing continuous suction, etc.
The use of digital drainage systems in general thoracic surgery is well known. Such systems are routinely used in adults in several countries, such as Italy and Germany; however, to our knowledge, there have been no reports on their use in pediatric thoracic surgery. This might be explained by the low incidence of prolonged air leak in children. As part of the protocol developed at our institution, we studied the usefulness of such a system also in children. The traditional water-seal drainage systems used in children are the same as those used in adults and have the same limitations regarding air leak.
In a digital system, air leak flow is quantified in mL/min and is also represented in graph format. The suction pres-sure is controlled by the system itself, which operates independently from the suction system of the hospital, and this provides autonomy and safety for patients and the health care team. In adults, the chest tube can be removed when the air leak flow is > 30 mL/min in the last 6 h, as displayed in the graph on the device screen .(2,4-7) For children, there are no established parameters; therefore, we defined an air leak flow < 10 mL/min in the last 6 h as the thresh-old for chest tube removal.
The system we studied was found to be functional, to be simple to use, and to offer new standards for thoracic drainage in pediatric surgery. It not only measured air leaks but also allowed early mobilization of patients, even for those on continuous suction, which is difficult to accomplish with a traditional system.(6,8)
Despite the lack of data on biosafety and thoracic drainage systems in the literature, subjective assessment by nursing staff was positive, being favored by an increase in practicality and the non-need for replacing the water seal daily. Because of minimal system handling, there is no risk of usual complications, such as lack of a water seal in the bottle, clamping of the system, chest tube disconnection or chest tube obstruction, etc. The system provided objective air leak data. Among the disadvantages is the fact that training is needed so that health care professionals can handle this new digital system and the fact that its cost is higher than that of a traditional system, mainly because of taxes and duties-the so called "custo Brasil" (cost of doing business in Brazil). To our knowledge, this is the first study on the use of this digital system in children. The digital drainage system facilitated the decision-making process during the postoperative period, thereby reducing the risk of errors in the interpretation and management of air leaks. Our study presents limited conclusions because it is a case series involving few patients. There is a need for further stud-ies on the use of digital drainage systems in children. Such studies should include devices that already are available in other countries and measure not only air leak but also fluid flow. The use of electronic health records is inevitable.
REFERENCES1. Costa Jr Ada S, Leão LE, Succi JE, Rymkiewicz E, Folador J, Kazantzis T. Digital drainage system: how far can we go? J Bras Pneumol. 2014;40(5):579-81. https://doi.org/10.1590/S1806-37132014000500015
2. Cerfolio RJ, Bryant AS. The benefits of continuous and digital air leak assessment after elective pulmonary resection: a prospective study. Ann Thorac Surg. 2008;86(2):396-401. https://doi.org/10.1016/j.athoracsur.2008.04.016
3. Ajami S, Bagheri-Tadi T. Barriers for Adopting Electronic Health Records (EHRs) by Physicians. Acta Inform Med. 2013;21(2):129-34. https://doi.org/10.5455/aim.2013.21.129-134
4. Mier JM, Molins L, Fibla JJ. The benefits of digital air leak assessment after pulmonary resection: prospective and comparative study [Article in Spanish]. Cir Esp. 2010,87(6):385-9. https://doi.org/10.1016/j.ciresp.2010.03.012
5. Cerfolio RJ, Varela G, Brunelli A. Digital and smart chest drainage systems to monitor air leaks: the birth of a new era? Thorac Surg Clin. 2010;20(3):413-20. https://doi.org/10.1016/j.thorsurg.2010.03.007
6. Bertolaccini L, Rizzardi G, Filice MJ, Terzi A. "Six Sigma approach" - an objective strategy in digital assessment of postoperative air leaks: a prospective randomized study. Eur J Cardiothorac Surg. 2011;39(5):e128-32. https://doi.org/10.1016/j.ejcts.2010.12.027
7. Pompili C, Detterbeck F, Papagiannopoulos K, Sihoe A, Vachlas K, Maxfield MW, et al. Multicenter international randomized comparison of objective and subjective outcomes between electronic and traditional chest drainage systems. Ann Thorac Surg. 2014;98(2):490-6; discussion 496-7. https://doi.org/10.1016/j.athoracsur.2014.03.043
8. Pompili C, Brunelli A, Salati M, Refai M, Sabbatini A. Impact of the learning curve in the use of a novel electronic chest drainage system after pulmonary lobectomy: a case-matched analysis on the duration of chest tube usage. Interact Cardiovasc Tho-rac Surg. 2011;13(5):490-3; discussion 493. https://doi.org/10.1510/icvts.2011.280941