ABSTRACT
The combination of tuberculosis with other diseases can affect tuberculosis treatment within populations. In the present study, social network analysis of data retrieved from the Mexican National Epidemiological Surveillance System was used in order to explore associations between the number of contacts and multimorbidity. The node degree was calculated for each individual with tuberculosis and included information from 242 contacts without tuberculosis. Multimorbidity was identified in 49.89% of individuals. The node degrees were highest for individuals with tuberculosis + HIV infection (p < 0.04) and lowest for those with tuberculosis + pulmonary edema (p < 0.07). Social network analysis should be used as a standard method for monitoring tuberculosis and tuberculosis-related syndemics.
Keywords:
Tuberculosis/epidemiology; HIV; Nutrition, public health.
RESUMO
A combinação de tuberculose e outras doenças pode afetar o tratamento da tuberculose nas populações. No presente estudo, a análise de redes sociais de dados extraídos do Sistema Nacional de Vigilância Epidemiológica do México foi usada para explorar as relações entre o número de contatos e a multimorbidade. O grau do nó foi calculado para cada indivíduo com tuberculose e incluiu informações a respeito de 242 contatos sem tuberculose. A multimorbidade foi identificada em 49,89% dos indivíduos. Os maiores graus dos nós foram os referentes a indivíduos com tuberculose + infecção pelo HIV (p < 0,04), e os menores foram os referentes a indivíduos com tuberculose + edema pulmonar (p < 0,07). A análise de redes sociais deve ser usada como método-padrão para monitorar a tuberculose e a sindemia relacionada com a tuberculose.
Palavras-chave:
Tuberculose/epidemiologia; HIV; Nutrição em saúde pública.
Tuberculosis is the second leading cause of death from an infectious disease worldwide, occurring primarily in developing countries.(1) In Mexico, the highest rates of morbidity and mortality from tuberculosis occur in only 0.95% of all municipalities, one of which is Hermosillo, the capital of the state of Sonora, in northwestern Mexico, near the United States-Mexico border. Spatial analysis has revealed clusters of tuberculosis cases there, in areas of high social deprivation.(2) Other risk factors for tuberculosis include belonging to an ethnic minority, consuming drugs or alcohol, having been in prison, being a panhandler, being HIV-positive, being male, and being young.(3) Transnational migration and the complex population dynamics of border areas such as the city of Hermosillo have also been considered particularly important, given that they can contribute to drug resistance.(4)
Although the associations between certain social determinants and the occurrence of tuberculosis have been explored,(5) the relationships among individuals have been less studied. Although one recent study explored social groups (social networks) among individuals with tuberculosis,(6) no social network analysis (SNA) methods were used. This type of analysis is important because it explores a new dimension of variables that goes beyond the traditional epidemiological approach based on the study of differences among persons, times, and places. SNA is the standard quantitative approach to the study of relationships among nodes, as in the case of individuals with tuberculosis. For instance, this methodology has been used in order to study how tuberculosis is transmitted during endemic and epidemic periods,(7-12) making it possible to identify the individuals and characteristics that facilitate transmission.
Tuberculosis has been reported in association with malnutrition, diabetes, smoking, alcoholism, chronic pulmonary disease, and HIV infection.(13,14) The combination of tuberculosis with other diseases, which is now known as "multimorbidity,"(15) is important because it can complicate clinical treatment and increase costs, among other reasons.(14) Given that previous social network analyses of individuals with tuberculosis have not addressed the topic of multimorbidity, the objective of the present study was to explore possible associations between the number of contacts and multimorbidity.
Epidemiological surveillance data for the city of Hermosillo were analyzed with the use of the Mexican National Epidemiological Surveillance System Integrated Information Platform (tuberculosis module). General data on patients registered with the Sonora State Medical Department were retrieved from the aforementioned system over a period of five months. In addition, reported data on contacts and comorbidities were collected for all patients admitted for medical examinations.
Some of the characteristics of the study participants were described by measures of central tendency and dispersion. A truth table was then constructed to describe the different presentations of multimorbidity in the individuals with tuberculosis. With those data, first-order egocentric social networks of individuals with tuberculosis were constructed; for those networks, a symmetric matrix was generated and subsequently converted into graphs with the program NetDraw, version 2.111.(16) The degree of each node in the network was then calculated with the program UCINET, version 6.232. (17) The degree of a node is a measure of centrality corresponding to the number of edges connected to a given node (i.e., its number of direct contacts).(18) Finally, the Mann-Whitney U test was used in order to compare the groups of individuals with and without each of the secondary diagnoses, the program Stata, version 13 (StataCorp LP, College Station, TX, USA), being used to that end.
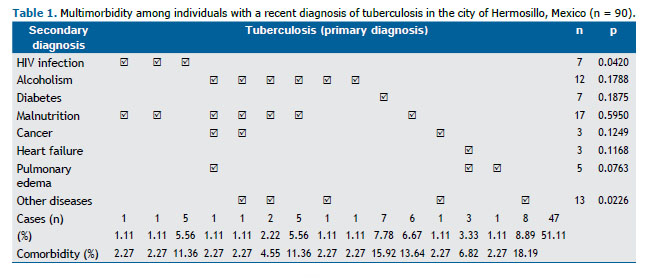
Of the individuals with tuberculosis (n = 90), most (76.67%) were male, whereas, of those without tuberculosis (n = 242), approximately half (50.40%) were female (p < 0.001). The individuals with tuberculosis varied widely in age (from 3 to 79 years), the median age being 30.5 years. Table 1 shows the distribution of multimorbidity among the individuals with tuberculosis, 49.89% of whom had tuberculosis and another disease. The most common comorbidities (and combinations of comorbidities) were diabetes, malnutrition, HIV infection, malnutrition + alcoholism, and heart failure + pulmonary edema, which together accounted for approximately three fifths of all comorbidities.
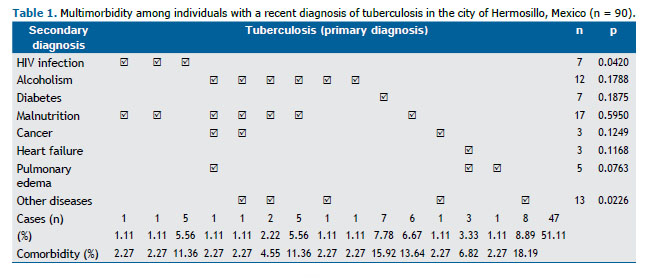
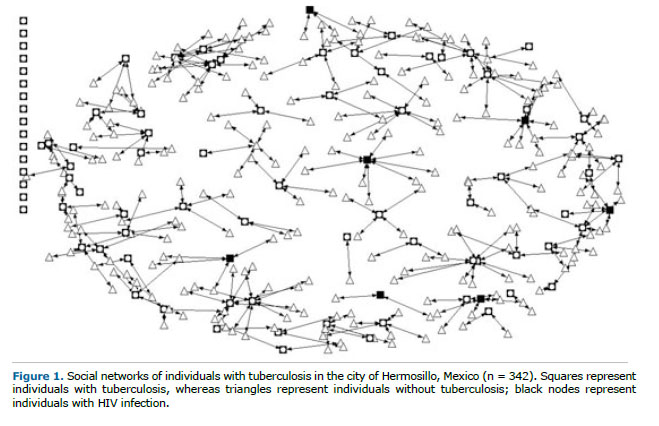
Figure 1 shows all first-order egocentric social networks of individuals with tuberculosis in the city of Hermosillo. The low density of the network is notable, as is the range of node degrees (from 0 to 9). A comparison of the node degrees for all types of multimorbidity (or lack thereof) revealed significant differences only between the node degree for tuberculosis + HIV infection and that for tuberculosis + pulmonary edema. The node degree for tuberculosis + HIV infection was higher than were those for tuberculosis + any other disease, whereas the node degree for tuberculosis + pulmonary edema was lower than was that for tuberculosis without pulmonary edema.
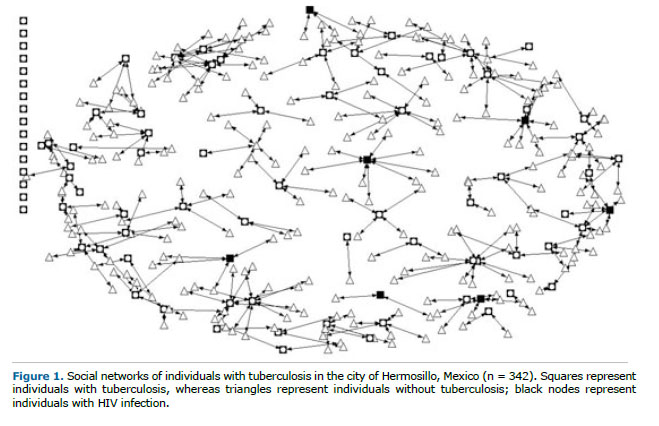
To the best of our knowledge, this study presents the first results of SNA of individuals with tuberculosis alone or in combination with other diseases in Mexico. Comorbidity was found to be common, and the most common comorbidities were malnutrition, alcoholism, HIV infection, and diabetes, findings that are consistent with the literature.(14) In addition, individuals with tuberculosis + HIV infection tended to have more contacts than did those with tuberculosis + any other disease, whereas the opposite was true for those with tuberculosis + pulmonary edema. On the basis of our data, this might be related to the age of the individuals with tuberculosis; those with tuberculosis + HIV infection tended to be younger, whereas those with tuberculosis + pulmonary edema tended to be older. Another possible explanation is that those with tuberculosis + HIV infection can easily live in the community while receiving treatment, whereas those with tuberculosis + pulmonary edema typically require hospital treatment and therefore become isolated from their social networks.
Some of the most important limitations of the present study are related to problems inherent to how data are collected in the Mexican National Epidemiological Surveillance System and the system protocols. The system is based on Official Mexican Standard NOM-017-SSA2-1994 and includes relatively few variables. In addition, the complete network was unavailable; only immediate (i.e., degree 1) networks were available. Given the cross-sectional design of the study, it was impossible to establish the temporality between the network of contacts and infection. This is important because differences in the number of contacts can reflect events that occurred before or after the diagnosis of tuberculosis or some of the concomitant diseases.
This is a pioneering study of multimorbidity and the social networks of individuals with tuberculosis. By incorporating the importance of the different positions and roles of individuals in their social relationships, it is possible to begin to go beyond the view of person-time-place variables as predictors of disease. This means that the analysis begins to change from one of comorbidity to one of syndemics. This term, coined by Merill Singer and Scott Clair,(19) makes it possible to describe the co-occurrence of diseases and their mutual reinforcement in epidemics or clusters. It also contributes to understanding their presence in terms of the consequences of social inequities and injustice. (20) This type of approach has been recommended to complement the conventional methods used for contact investigations,(11) and surveillance systems should therefore incorporate social network tools as a first step toward exploring nonbiological determinants.
REFERENCES1. Falzon D, Mirzayev F, Wares F, Baena IG, Zignol M, Linh N, et al. Multidrug-resistant tuberculosis around the world: what progress has been made? Eur Respir J. 2015;45(1):150-60. http://dx.doi.org/10.1183/09031936.00101814
2. Alvarez-Hernández G, Lara-Valencia F, Reyes-Castro PA, Rascón-Pacheco RA. An analysis of spatial and socio-economic determinants of tuberculosis in Hermosillo, Mexico, 2000-2006. Int J Tuberc Lung Dis. 2010;14(6):708-13.
3. Nava-Aguilera E, Andersson N, Harris E, Mitchell S, Hamel C, Shea B, et al. Risk factors associated with recent transmission of tuberculosis: systematic review and meta-analysis. Int J Tuberc Lung Dis. 2009;13(1):17-26.
4. Fitchett JR, Vallecillo AJ, Espitia C. Tuberculosis transmission across the United States-Mexico border. Rev Panam Salud Publica. 2011;29(1):57-60. http://dx.doi.org/10.1590/S1020-49892011000100009
5. Marais BJ, Hesseling AC, Cotton MF. Poverty and tuberculosis: is it truly a simple inverse linear correlation? Eur Resp J. 2009;33(4):943-44. http://dx.doi.org/10.1183/09031936.00173608
6. Peñuelas-Urquides K, Martínez-Rodríguez HG, Enciso-Moreno JA, Molina-Salinas GM, Silva-Ramírez B, Padilla-Rivas GR, et al. Correlations between major risk factors and closely related Mycobacterium tuberculosis isolates grouped by three current genotyping procedures: a population-based study in northeast Mexico. Mem Inst Oswaldo Cruz. 2014;109(6):814-819. http://dx.doi.org/10.1590/0074-0276130550
7. McElroy PD, Rothenberg RB, Varghese R, Woodruff R, Minns GO, Muth SQ, et al. A network-informed approach to investigating a tuberculosis outbreak: implications for enhancing contact investigations. Int J Tuberc Lung Dis. 2003;7(12 Suppl 3):S486-93.
8. Cook VJ, Sun SJ, Tapia J, Muth SQ, Arguello DF, Lewis BL, et al. Transmission network analysis in tuberculosis contact investigations. J Infect Dis. 2007;196(10):1517-27. http://dx.doi.org/10.1086/523109
9. Gardy JL, Johnston JC, Ho Sui SJ, Cook VJ, Shah L, Brodkin E, et al. Whole-genome sequencing and social-network analysis of a tuberculosis outbreak. N Engl J Med. 2011;364(8):730-9. http://dx.doi.org/10.1056/NEJMoa1003176
10. Cook VJ, Shah L, Gardy J, Bourgeois AC. Recommendations on modern contact investigation methods for enhancing tuberculosis control. Int J Tuberc Lung Dis. 2012;16(3):297-305. http://dx.doi.org/10.5588/ijtld.11.0350
11. Cook VJ, Shah L, Gardy J. Modern contact investigation methods for enhancing tuberculosis control in aboriginal communities. Int J Circumpolar Health. 2012;71:18643. http://dx.doi.org/10.3402/ijch.v71i0.18643
12. Kawatsu L, Izumi K, Uchimura K, Urakawa M, Ohkado A, Takahashi I. Can social network analysis assist in the prioritisation of contacts in a tuberculosis contact investigation? Int J Tuberc Lung Dis. 2015;19(11):1293-9. http://dx.doi.org/10.5588/ijtld.15.0378
13. Bates M, Marais BJ, Zumla A. Tuberculosis Comorbidity with Communicable and Noncommunicable Diseases. Cold Spring Harb Perspect Med. 2015;5(11). pii: a017889. http://dx.doi.org/10.1101/cshperspect.a017889
14. Marais BJ, Lönnroth K, Lawn SD, Migliori GB, Mwaba P, Glaziou P, et al. Tuberculosis comorbidity with communicable and non-communicable diseases: integrating health services and control efforts. Lancet Infect Dis. 2013;13(5):436-48. http://dx.doi.org/10.1016/S1473-3099(13)70015-X
15. Fernández-Niño JA, Bustos-Vázquez E. Multimorbidity: conceptual basis, epidemiological models and measurement challenges. Biomedica. 2016;36(2):188-203.
16. Borgatti SP. NetDraw: Graph visualization software. Harvard, MA: Harvard Analytic Technologies; 2002.
17. Borgatti SP, Everett MG, Freeman LC. Ucinet for Windows: Software for social network analysis. Harvard, MA: Harvard Analytic Technologies; 2002.
18. Freeman LC. Centrality in social networks conceptual clarification. Social Networks. 1978-9;1(3):215-39.
19. Singer M, Clair S. Syndemics and public health: reconceptualizing disease in bio-social context. Med Anthropol Q. 2003;17(4):423-41. http://dx.doi.org/10.1525/maq.2003.17.4.423
20. Littleton J, Park J. Tuberculosis and syndemics: Implications for Pacific health in New Zealand. Soc Sci Med. 2009;69(11):1674-80. http://dx.doi.org/10.1016/j.socscimed.2009.08.042