AO EDITOR, A Doença do Coronavírus 2019 (COVID-19) surgiu como um grave problema de saúde pública em todo o mundo. (1) Até o momento, mais de 31 milhões de casos e quase 669.000 mortes por COVID-19 foram confirmados no Brasil. Os maiores custos e taxas de mortalidade foram atribuídos a pacientes idosos gravemente doentes com comorbidades submetidos a ventilação mecânica invasiva (VMI).(2) Diversos tratamentos e medidas preventivas foram usadas, como o uso de máscaras faciais, o distanciamento social, a higiene rigorosa das mãos, medicamentos, e vacinas contra a síndrome respiratória aguda grave por Coronavírus 2 (SARS-CoV-2), mas qual delas foi a melhor em reduzir o número de casos e as taxas de mortalidade?
Após a implementação dos programas de vacinação em dezembro em Israel(3) e Inglaterra,(4) houve uma redução significativa no número de casos sintomáticos e assintomáticos, internações, doença grave e óbitos por COVID-19. No Brasil, o programa de vacinação contra o SARS-CoV-2 foi iniciado em 17 de janeiro de 2021, priorizando profissionais de saúde e a população idosa com comorbidades. Até 26 de junho de 2021, 11,92% da população brasileira estava completamente vacinada e 33,21% receberam apenas uma dose; esse período foi o pior em termos de número de casos e letalidade em 2021, principalmente nas faixas etárias mais jovens.(5) Desta forma, na presente carta, objetivamos comparar as mudanças nas taxas de mortalidade e na epidemiologia da COVID-19 em pacientes graves antes e depois dos primeiros 6 meses após o programa de vacinação contra SARS-CoV-2 no Brasil.
Este estudo retrospectivo analisou os dados de pacientes adultos com COVID-19 internados em unidades de terapia intensiva (UTIs) no Brasil. Os pacientes foram incluídos quando a infecção por SARS-CoV-2 foi confirmada por teste de reação em cadeia da polimerase em tempo real (RT-PCR). A aprovação do comitê de ética não foi necessária, pois os dados foram obtidos de um registro nacional do Sistema de Informação da Vigilância Epidemiológica da Gripe (SIVEP-Gripe), disponível online pelo site https://covid.saude.gov.br.
Os pacientes graves com COVID-19 foram divididos em dois grupos de acordo com a data de internação. Aqueles internados entre 1 de março e 31 de dezembro de 2020 foram incluídos no grupo do período pré-vacinação, enquanto os internados entre 1 de janeiro e 26 de junho de 2021 foram incluídos no grupo do período pós-vacinação. As variáveis avaliadas mensalmente foram a média de idade, a frequência de pacientes sem comorbidades e a taxa de mortalidade.
Os dados foram analisados por meio do software SPSS, versão 27.0. Foi realizada uma análise descritiva da população do estudo usando medidas de média e desvio padrão como variáveis contínuas e distribuição de frequência absoluta e relativa como variáveis categóricas. O teste t foi utilizado para comparar variáveis contínuas, enquanto o teste qui-quadrado foi realizado para comparar variáveis categóricas. As diferenças foram consideradas significantes quando o valor de p era < 0,05.
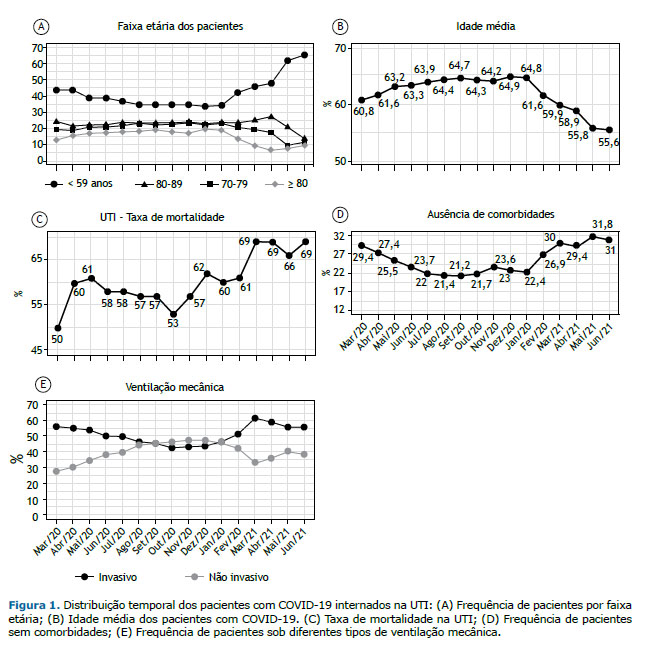
Este estudo avaliou um total de 116.640 pacientes internados na UTI no período pré-vacinal e 124.153 pacientes internados no período pós-vacinal, dos quais 68.052 (58,3%) e 82.402 (66,4%) foram a óbito, respectivamente. Após o programa de vacinação contra SARS-CoV-2, os pacientes graves com COVID-19 foram comparados com os do período pré-vacinação. A frequência de infecção entre os pacientes < 60 anos aumentou e a média de idade dos pacientes diminuiu, principalmente após o período vacinal quando comparado ao grupo do período pré-vacinal (Figuras 1A e 1B). No entanto, houve tendências temporais de aumento da taxa de mortalidade na UTI, da frequência de pacientes sem comorbidades e da necessidade de VMI (Figuras 2A, 2B e 2C).
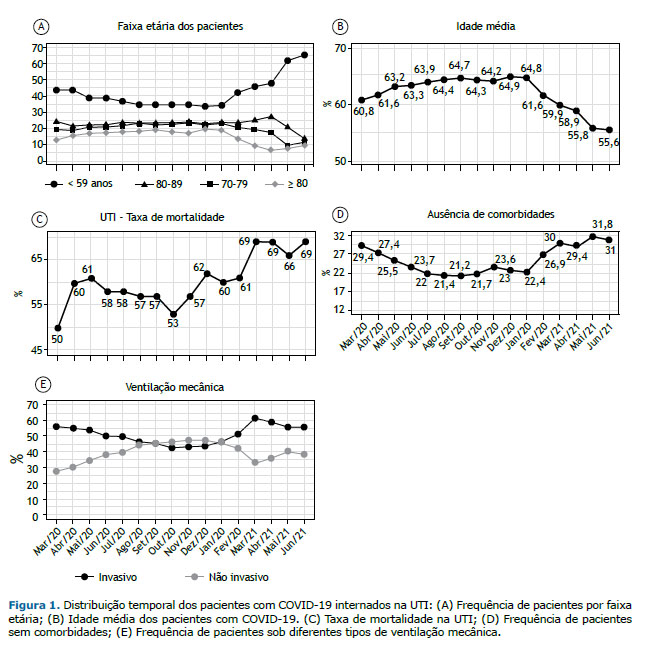
O presente estudo identificou mudanças consistentes nos perfis de faixa etária em pacientes graves confirmados com COVID-19 após o programa de vacinação contra SARS-CoV-2 no Brasil. Pacientes com menos de 60 anos de idade tornaram-se o grupo que foi mais frequentemente internado na UTI, com aumento das taxas de mortalidade na UTI e da necessidade de VMI. Tal resultado sugere fortemente que as vacinas contra SARS-CoV-2 protegem a população brasileira e devem ser amplamente oferecidas a todas as faixas etárias, incluindo crianças e adolescentes.
Alguns medicamentos mostraram efeitos benéficos no tratamento de pacientes graves com COVID-19. A dexametasona apresentou uma razão de taxa de 0,83 (IC95%, 0,75–0,93) para todos os pacientes hospitalizados e 0,64 (0,51–0,81), especialmente para pacientes submetidos a ventilação invasiva. (6) Bloqueadores de receptores de interleucina-6 (tocilizumab, sarilumab) também promoveram uma diminuição da mortalidade,(7) embora seus altos custos dificultem a disponibilidade para o tratamento de pacientes principalmente no sistema público de saúde. Além disso, mais conhecimento sobre a COVID-19, principalmente o uso de ventilação não invasiva e invasiva, poderia melhorar a qualidade da assistência à saúde.(8)
A Organização Mundial da Saúde (OMS) e todas as sociedades médicas sugeriram que todos sejam vacinados o mais rápido possível. Diferentes vacinas contra SARS-CoV-2 têm sido consideradas eficazes e seguras.(3,4,9) Os desfechos mais importantes relacionados à eficácia de uma vacina são a capacidade de reduzir internações hospitalares ou de cuidados intensivos e/ou o óbito.(10) Nosso estudo identificou mudanças na frequência das faixas etárias de pacientes graves com COVID-19 após o programa de vacinação, especificamente em adultos mais velhos vacinados, que apresentaram redução na frequência de admissão na UTI. Portanto, pode-se inferir que o programa de vacinação contra SARS-CoV-2 foi a medida mais importante para o controle da pandemia de COVID-19.
As taxas de frequência e mortalidade por COVID-19 foram muito mais descontroladas até o 1º semestre de 2021 no Brasil. A variante Gama de SARS-CoV-2 foi predominante nesse período e relacionada a maior gravidade e mortalidade, principalmente em faixas etárias mais jovens quando comparadas às variantes B.1.1.28 e B.1.1.33, que foram as mais prevalentes em 2020 no Brasil.(5) Nosso estudo mostrou que pacientes abaixo de 60 anos aumentaram as taxas de mortalidade na UTI devido ao fato de os idosos serem prioridade para a vacinação. Esse achado é preocupante uma vez que a população mais jovem é economicamente ativa e provavelmente responsável pelas obrigações financeiras de suas famílias e empresas trabalhistas. Desta forma, podemos inferir que a variante Gama teve maior capacidade de propagação do que as demais variantes. No entanto, ocorreu principalmente entre os mais jovens, pois ainda não haviam sido vacinados.
Em conclusão, este estudo identificou uma mudança importante na frequência da faixa etária de pacientes graves com COVID-19, diminuindo na população mais velha após o programa de vacinação contra SARS-CoV-2 no Brasil. Embora tais achados sugiram que a distribuição da vacina tenha evitado novas internações em cuidados intensivos, especialmente nos grupos prioritários que foram vacinados, houve preocupação com o aumento das taxas de mortalidade na UTI e/ou necessidade de VMI, o que afetou principalmente pacientes mais jovens por ainda não terem sido vacinados. Investir em vacinas contra SARS-CoV-2 foi a forma mais rápida e adequada de controlar essa terrível pandemia de COVID-19, que, infelizmente, ainda está em andamento.
AGRADECIMENTOS Gostaríamos de expressar nossa gratidão e respeito a todas as famílias brasileiras que perderam parentes durante a pandemia de COVID-19. Queremos também parabenizar todos os profissionais de saúde que trabalharam incansavelmente pela recuperação de todos os pacientes com COVID-19. Por fim, agradecemos à equipe do Sistema de Informação da Vigilância Epidemiológica da Gripe (SIVEP-Gripe) pela disponibilização da base de dados utilizada online e de domínio público; este estudo não teria sido possível sem esta organização e os dados dela obtidos.
REFERÊNCIAS 1. WHO Coronavirus (COVID-19) Dashboard_WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. Available from: https://covid19.who.int/.
2. Ranzani OT, Bastos LSL, Gelli JGM, Marchesi JF, Baião F, Hamacher S, et al. Characterisation of the first 250,000 hospital admissions for COVID-19 in Brazil: a retrospective analysis of nationwide data. Lancet Respir Med. 2021;9(4):407-418. https://doi.org/10.1016/S2213-2600(20)30560-9.
3. Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel : an observational study using national surveillance data. Lancet. 2021;397(10287):1819–29. https://doi.org/10.1016/S0140-6736(21)00947-8.
4. Lopez Bernal J, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. BMJ. 2021;373:n1088. https://doi.org/10.1136/bmj.n1088.
5. Zeiser FA, Donida B, da Costa CA, Ramos GO, Scherer JN, Barcellos NT, et al. First and second COVID-19 waves in Brazil: A cross-sectional study of patients’ characteristics related to hospitalization and in-hospital mortality. Lancet Reg Health Am. 2022;6:100107. https://doi.org/10.1016/j.lana.2021.100107.
6. RECOVERY Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, et al. Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 2021;384(8):693–704. https://doi.org/10.1056/NEJMoa2021436.
7. World Health Organization. Therapeutics and COVID-19: living guideline. World Heal Organ. 2022;10th editi(22 April):1–128.
8. Braz Júnior DDS, de Mello MJG, Lyra NABE, Viana MMA, Borba VS, Thuler LCS, et al. Letter from Brazil. Respirology. 2021;26(11):1085-87. https://doi.org/10.1111/resp.14164.
9. Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021;384(5):403–16. https://doi.org/10.1056/NEJMoa2035389.
10. Hodgson SH, Mansatta K, Mallett G, Harris V, Emary KRW, Pollard AJ. What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical effi-cacy of vaccines against SARS-CoV-2. Lancet Infect Dis. 2021;21(2):e26–e35. https://doi.org/10.1016/S1473-3099(20)30773-8.