ABSTRACT
Objective: Mobile health (mHealth) applications are scarce for children and adolescents with chronic pulmonary diseases (CPDs). This study aimed to map and describe the contents of the mHealth apps available for use in children and adolescents with CPDs. Methods: We performed a systematic mapping review of published scientific literature in PubMed, Scopus, and Cochrane Library by February of 2023, using relevant keywords. Inclusion criteria were as follows: children aged < 18 years with CPDs; and studies published in English on mHealth apps. Results: A total number of 353 studies were found, 9 of which met the inclusion criteria. These studies described seven mHealth apps for Android and iOS, designed either for asthma (n = 5) or for cystic fibrosis (n = 2). Five content areas were identified: education/information; pharmacological treatment; emergency; support; and non-pharmacological treatment. The studies (4, 2, and 3, respectively) showed consistent findings using qualitative, quantitative, and mixed methodologies. Conclusions: This mapping review provided a guided selection of the most appropriate mHealth apps for use in children and adolescents with CPDs based on the needs of each target population. However, these mHealth apps have limited capabilities to reinforce disease self-management and provide information related to treatment compliance.
Keywords:
Lung diseases; Child, Adolescent; Treatment adherence and compliance; Telemedicine; Self-management.
RESUMO
Objetivo: Aplicativos de saúde móvel (mHealth, do inglês mobile health) para crianças e adolescentes com doenças pulmonares crônicas (DPC) são escassos. Este estudo teve como objetivo mapear e descrever o conteúdo dos aplicativos de mHealth disponíveis para uso em crianças e adolescentes com DPC. Métodos: Realizamos uma revisão sistemática de mapeamento da literatura científica publicada nos bancos de dados PubMed, Scopus e Cochrane Library até fevereiro de 2023, utilizando descritores relevantes. Os critérios de inclusão foram os seguintes: crianças menores de 18 anos com DPC e estudos publicados em inglês sobre aplicativos de mHealth. Resultados: Foram encontrados 353 estudos, dos quais 9 atenderam aos critérios de inclusão. Esses estudos descreveram sete aplicativos de mHealth para Android e iOS projetados para asma (n = 5) ou para fibrose cística (n = 2). Foram identificadas cinco áreas de conteúdo: educação/informação, tratamento farmacológico, emergência, suporte e tratamento não farmacológico. Os estudos (4, 2 e 3, respectivamente) apresentaram achados consistentes utilizando metodologias qualitativas, quantitativas e mistas. Conclusões: Esta revisão de mapeamento forneceu uma seleção guiada dos aplicativos de mHealth mais adequados para uso em crianças e adolescentes com DPC com base nas necessidades de cada população-alvo. No entanto, esses aplicativos de mHealth têm capacidades limitadas para reforçar a autogestão da doença e fornecer informações relacionadas à adesão ao tratamento.
Palavras-chave:
Doenças pulmonares; Criança; Adolescente; Cooperação e adesão ao tratamento; Telemedicina; Autogestão.
INTRODUÇÃO Em pediatria, a gestão eficaz da doença inclui tomar os medicamentos prescritos, comparecer a consultas médicas, automonitorar sintomas, identificar e minimizar exposições a gatilhos ambientais, aderir a um plano de ação personalizado e comunicar-se com os profissionais de saúde sobre sintomas e tratamentos.(1) Tradicionalmente, as consultas clínicas servem de cenário principal para que os pacientes pediátricos recebam educação sobre a doença e suporte para a autogestão. No entanto, cada vez mais as crianças e os cuidadores buscam informações e assistência autogerenciáveis, sendo direcionados para formas alternativas de suporte como o uso de sites relevantes e de aplicativos de saúde móvel (mHealth, do inglês mobile health).(2)
O uso de telefones celulares está aumentando rapidamente em todo o mundo.(3) Em 2019, quase 46% das crianças entre 5 e 17 anos de idade na Europa tinham um smartphone, sendo que 41% delas o utilizavam diariamente.(4) Essa nova realidade propiciou a adoção dessa tecnologia para dar suporte a serviços de prática médica e de saúde pública.(5) Portanto, os aplicativos de mHealth tornaram-se uma ferramenta promissora para o fornecimento de suporte a crianças e cuidadores a fim de que possam gerenciar esquemas terapêuticos e sintomas, tendo como objetivo aprimorar a autogestão de doenças crônicas e, consequentemente, melhorar a qualidade de vida desses pacientes. Os aplicativos criados para a gestão de doenças pulmonares crônicas (DPC) geralmente incluem funções como lembretes por escrito, informações sobre a ingestão de medicamentos, registros de sintomas e monitoramento da função pulmonar, bem como educação sobre a patologia da doença.(2,6-9)
Além dessa tentativa, as informações trocadas entre pacientes e médicos clínicos (como relatórios de pré-consulta dos pacientes em arquivo PDF (Adobe Acrobat) antes da consulta clínica) podem ser ampliadas pela tecnologia de mHealth. Em outras palavras, essa tecnologia pode facilitar a estimativa dos sintomas e a modificação dos esquemas de tratamento farmacológico e não farmacológico quando necessário, bem como o processo de detecção de uma exacerbação da doença. (2,8) Embora os aplicativos de mHealth sejam projetados de forma ideal para fornecer suporte na autogestão da doença e para empoderar os indivíduos para que adiram ao tratamento, pouquíssimos aplicativos foram investigados quanto ao seu impacto nos resultados clínicos.
Este artigo de revisão tem como objetivo mapear e classificar os estudos existentes sobre aplicativos de mHealth projetados para serem utilizados na gestão farmacológica e não farmacológica de DPC em crianças e adolescentes. Reconhecendo alguns limites na classificação dos aplicativos existentes, os médicos clínicos podem tomar decisões baseadas em evidências sobre qual aplicativo é o mais adequado para uso ou podem sugerir novos campos de interesse ao perceberem quaisquer lacunas de pesquisa.
MÉTODOS Delineamento do estudo Utilizou-se uma metodologia de revisão sistemática de mapeamento para encontrar estudos publicados sobre aplicativos de mHealth projetados para a autogestão de DPC em crianças e adolescentes.(10) Nossa abordagem foi baseada nos princípios definidos pelo Social Care Institute for Excellence.(11) O mapa sistemático vem sendo cada vez mais utilizado em pesquisas sobre serviços de saúde as quais têm como objetivo mapear e categorizar um tema na literatura para a realização de trabalhos novos e mais detalhados.(10) Esse método é útil para resumir e organizar uma ampla e heterogênea base de evidências a fim de identificar investigações mais específicas.(11) O protocolo foi registrado na plataforma Open Science Framework (https://doi.org/10.17605/OSF.IO/ADKGF), já que o International Prospective Register of Systematic Reviews atualmente não está aceitando registros para revisões de mapeamento.
Critérios de elegibilidade Os critérios de inclusão foram artigos publicados na língua inglesa até fevereiro de 2023. Foram incluídos nesta revisão estudos sobre crianças com DPC (como asma, fibrose cística e bronquiectasia não fibrocística) com menos de 18 anos de idade e que utilizavam aplicativos de mHealth com abordagem comportamental de fácil utilização. Foram excluídos resumos, resenhas de livros, capítulos de livros, revisões narrativas, estudos pré-clínicos, revisões de escopo, revisões sistemáticas, meta-análises, séries/relatos de caso, comentários, cartas ao editor, editoriais, diretrizes de prática clínica, protocolos e estudos cujos textos completos não estavam disponíveis. Além disso, foram excluídos estudos relacionados a adultos ou a outras doenças pediátricas crônicas ou agudas (como doenças musculoesqueléticas e neurológicas) ou cujo processo de pesquisa para o desenvolvimento do aplicativo de mHealth e as intervenções não tivessem sido descritos. Nesta revisão de mapeamento, optou-se por não buscar relatos não publicados e a literatura cinzenta.
Estratégia de busca Uma busca sistemática da literatura foi realizada em três bancos de dados (PubMed, Scopus e Cochrane Library) até fevereiro de 2023 por um dos pesquisadores (VS). A estratégia de busca foi elaborada utilizando descritores e termos MeSH relacionados a aplicativos de mHealth, tratamento farmacológico/não farmacológico, crianças/adolescentes e DPC (Material suplementar).
Triagem e seleção de artigos Os estudos foram avaliados para inclusão por meio da revisão dos títulos e resumos. Os resultados da busca foram exportados para o Endnote X9 (Clarivate, Filadélfia, PA, EUA). Após a exclusão das duplicatas, dois investigadores (VS e PK) avaliaram de forma independente os títulos, resumos e textos completos dos estudos para tomar uma decisão final. Foram excluídos os estudos que não atenderam aos critérios de elegibilidade. Em seguida, realizou-se uma busca secundária a partir de citações nos artigos incluídos e em revisões anteriores sobre o uso de aplicativos de mHealth. Buscaram-se os textos completos de todos os estudos relevantes, que foram baixados e avaliados adicionalmente quanto ao cumprimento dos critérios de elegibilidade. Em caso de discordância, um terceiro revisor (EK) foi consultado para tomar a decisão final, garantindo assim a minimização de vieses na decisão de incluir ou não um estudo. Por fim, todos os membros da equipe de pesquisa decidiram por consenso sobre a inclusão dos estudos selecionados.
Extração de dados Diante dos relativamente poucos estudos relevantes na literatura, decidimos incluir estudos com diferentes metodologias. Um modelo incluindo a metodologia do estudo, local do estudo, ano de publicação e principais perspectivas foi desenvolvido para orientar a extração de dados. VS e EP extraíram de forma independente os dados dos artigos incluídos, e EK realizou a verificação final. Qualquer discordância foi discutida e resolvida por consenso.
Com base em Fernández-Sotos et al.,(12) um aspecto metodológico fundamental para uma revisão sistemática de mapeamento bem-sucedida é a definição das questões de pesquisa (QP) a serem respondidas. Portanto, as QP selecionadas nesta revisão de mapeamento foram as seguintes:
- QP1: Quais são os aplicativos de mHealth disponíveis para uso em crianças e adolescentes com DPC?
- QP2: Qual é o conteúdo de cada aplicativo de mHealth?
Risco de viés/qualidade dos estudos O principal objetivo de uma revisão sistemática de mapeamento é descrever o que há de mais moderno sobre o tema.(11) O risco de viés é determinado de forma genérica pela classificação do tipo de estudo. Esta revisão sistemática de mapeamento foi realizada para fornecer uma visão geral dos aplicativos de mHealth existentes, independentemente da qualidade metodológica ou do risco de viés derivado de cada estudo. Portanto, as fontes de evidências não são avaliadas criticamente e foram revisadas quanto à coerência da pesquisa e à utilidade dos achados referentes ao foco principal da pesquisa.(12)
RESULTADOS Fluxo de estudos A estratégia de busca eletrônica identificou 353 artigos relevantes. Após a remoção das duplicatas, 164 estudos foram revisados pelo título e resumo, sendo que 129 estudos foram excluídos. Dos 35 estudos com texto completo avaliados quanto à elegibilidade, 9 foram incluídos para estudo adicional. A Figura 1 apresenta o fluxograma do processo de seleção de estudos realizado de acordo com as recomendações do Preferred Reporting Items for
Systematic Reviews and Meta-Analyses.
Características dos estudos selecionados A Tabela 1 fornece um resumo das características dos estudos incluídos. Quatro estudos foram conduzidos com base em métodos qualitativos,(2,8,13,14) dois eram estudos descritivos quantitativos,(15,16) e três estudos adotaram métodos mistos de pesquisa.(7,17,18) Quatro, dois e três estudos, respectivamente, foram realizados na Europa,(2,7,8,16) EUA,(14,15) e Austrália(13,17,18) entre 2017 e 2022. Quatro dos estudos utilizaram uma amostra de pacientes pediátricos com DPC,(2,13,15,16) outros dois estudos utilizaram uma amostra composta por todas as partes interessadas (pacientes, profissionais de saúde [PS] e pais),(8,14) e um estudo utilizou uma amostra de PS e cuidadores de crianças com asma dos povos originários australianos (Australian First Nations Health and Care).(18) Além disso, um estudo utilizou uma amostra composta por aplicativos de mHealth,(7) e outro estudo utilizou uma amostra composta por estudantes.(17)

Entre os estudos incluídos na presente revisão sistemática de mapeamento, foram mencionados sete aplicativos específicos de mHealth(7) (Tabela 2). Em detalhe, dois dos estudos revisados avaliaram um aplicativo chamado Genia, direcionado a pacientes com fibrose cística (FC).(2,14) Dois estudos examinaram o aplicativo de mHealth chamado MyCyFAPP, desenvolvido como uma ferramenta de autogestão para pacientes com FC e seus familiares.(8,16) Além disso, cinco aplicativos (para iOS e Android) eram direcionados a pacientes com asma: Kiss my Asthma; Ask Me, AsthMe!; ASTHMAXcel; Asthma First Aid; e Menzies Asthma.(7,13,15,17,18)

O aplicativo Genia foi projetado para iOS e tem como objetivo promover a colaboração entre pacientes com FC (média de idade = 17,8 anos), familiares e equipes de saúde, com especial enfoque em dar às crianças e adolescentes um papel central no processo decisório. O aplicativo foi criado pela Upstream Dream, empresa sediada na Suécia, sendo um projeto de financiamento colaborativo com a Genentech. Como plataforma e como sistema de suporte ao paciente baseado em aplicativo, o aplicativo Genia enfatiza a participação do usuário, o fornecimento de feedback e a formação colaborativa de conteúdo. A principal funcionalidade do sistema foi encomendada como parte de uma iniciativa de aprendizagem colaborativa relacionada a um microssistema clínico especial, chamado Lund Pediatric Cystic Fibrosis. Isso envolveu médicos clínicos, pesquisadores, familiares e pacientes com FC para a determinação do conteúdo do aplicativo, sendo que as principais funções foram otimizadas e inspiradas pelos pacientes.(2,14)
O MyCyFAPP foi projetado para Android para ser utilizado por crianças e adolescentes com FC (< 18 anos de idade), familiares e PS, que podem gerenciar o tratamento da doença de forma conjunta e ininterrupta. O projeto multidisciplinar (denominado Horizonte 2020, que se estendeu por quatro anos — de 1º de janeiro de 2015 a 31 de dezembro de 2018) foi criado e financiado pelo European Commission Framework Program for Research and Innovation. Pacientes e familiares podem contar com o aplicativo para autogerenciar a nutrição e outros aspectos do tratamento não farmacológico e farmacológico. Os PS utilizam essa ferramenta para monitorar e acompanhar o progresso dos pacientes, garantindo feedback entre as duas partes quando julgado necessário.(8,16)
O aplicativo Kiss my Asthma foi desenvolvido por uma equipe de pesquisadores da Universidade de Sydney, do Instituto Woolcock de Pesquisa Médica e da Universidade de Melbourne com recursos provenientes do Asthma Australia’s National Research Fund. O aplicativo está disponível nas plataformas iOS e Android e fornece aos usuários (< 18 anos de idade) acesso conveniente ao plano de ação para asma, lembretes de medicamentos, dicas sobre como evitar gatilhos e estratégias para o controle da asma. Além disso, o aplicativo oferece recursos educacionais sobre asma e permite que os usuários definam metas pessoais. Ao fazer pequenas alterações, os usuários podem reduzir a frequência das crises de asma e melhorar o controle geral da asma. O objetivo final do aplicativo é ajudar os usuários a levar uma vida normal e não permitir que os sintomas da asma afetem suas atividades diárias.(13)
O aplicativo Ask Me, AsthMe! foi projetado para iOS para ajudar crianças (12-18 anos de idade) e familiares a aumentar seus conhecimentos sobre a asma pediátrica e controlar os sintomas da asma de forma eficaz. O aplicativo foi criado pela New York City Health and Hospitals Corporation sem qualquer financiamento. É um aplicativo com diversas funções que têm como objetivo ajudar o usuário a compreender a asma infantil e os parâmetros da asma. De fato, o aplicativo foi avaliado positivamente e considerado capaz de contribuir para a gestão da asma infantil.(7)
O ASTHMAXcel é um aplicativo personalizado e baseado em evidências para a gestão dos sintomas da asma, desenvolvido por uma equipe de médicos especialistas em asma, programadores de software e cientistas comportamentais. O trabalho foi financiado pelo Prêmio de Pesquisa em Doenças Respiratórias Alérgicas, patrocinado pela American Lung Association e pela American Academy of Allergy, Asthma and Immunology Foundation. O projeto foi financiado por meio de bolsa de serviços comunitários concedida pelo Stony Wold-Herbert Fund e de bolsa de pesquisa concedida pela Genentech. Como parte do programa ASTHMAXcel, foi desenvolvido um aplicativo móvel em forma de jogo chamado ASTHMAXcel Adventures para crianças e adolescentes com asma (7-17 anos de idade), disponível nas plataformas iOS e Android. O aplicativo apresenta vídeos curtos e jogos interativos educacionais que combinam animação com contação de histórias informativas. Possui uma tela introdutória com cinco níveis para o usuário escolher. Cada nível é composto por um a três vídeos tutoriais e jogos correspondentes que exigem que os usuários respondam a perguntas relacionadas aos vídeos.(15)
O aplicativo Asthma First Aid é uma ferramenta útil em situações de emergência em asma, disponível nas plataformas iOS e Android. Foi criado pelo Asthma Australia (Centro de Excelência em Pesquisa em Saúde Pulmonar do Conselho Nacional de Saúde e Pesquisa Médica da Austrália) como uma ferramenta educacional para crianças com asma (12-18 anos de idade), familiares e cuidadores, proporcionando fácil acesso às etapas de resposta a emergências. Abrange os primeiros socorros em caso de emergência em asma, além da capacidade de revisar cada uma das quatro etapas dos primeiros socorros.(17)
O aplicativo Menzies Asthma é um aplicativo multilíngue específico para os povos originários, baseado no atual flipchart pictórico da asma pediátrica, com “locução” em sete línguas dos povos originários e em inglês. Esse projeto foi financiado pelo Asthma Australia e foi produzido pela Divisão de Saúde Infantil da Menzies School of Health Research. Utiliza imagens interativas, áudio e quizzes para ensinar crianças (4-18 anos de idade) sobre a asma. É um método inovador e culturalmente aceitável de fornecer educação em saúde respiratória baseada em evidências para populações cultural e linguisticamente diversas entre os povos originários da Austrália.(18)
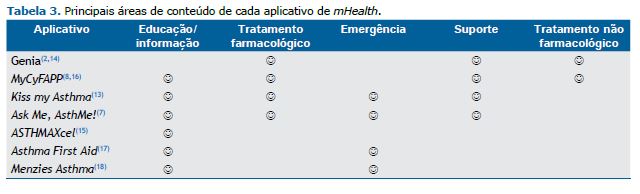
QP2: Qual é o conteúdo de cada aplicativo de mHealth? A Tabela 3 apresenta os principais aspectos pesquisados em relação ao conteúdo de cada aplicativo. Foram identificadas cinco principais áreas de conteúdo: educação/informação, tratamento farmacológico, emergência, suporte e tratamento não farmacológico.
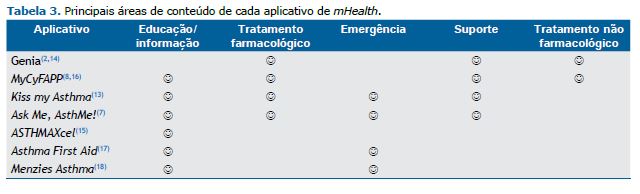
Seis dos aplicativos incluídos oferecem informações sobre a doença por meio de vídeos educacionais, contribuindo para a autogestão da doença e melhorando a formação cognitiva tanto das crianças quanto dos pais. (7,8,13,15-18) Quatro aplicativos funcionam como diários farmacológicos.(2,7,8,13,14,16) Além disso, quatro aplicativos indicam procedimentos de emergência para pacientes pediátricos com crises de asma.(7,13,17,18) Informações sobre sintomas e lembretes de medicamentos são fornecidos em quatro aplicativos.(2,7,8,13,14,16) Por fim, dois dos aplicativos podem fornecer elementos não farmacológicos com foco nos aspectos nutricionais de crianças com FC e na adesão à realização de exercícios de fisioterapia respiratória por meio da pontuação na escala de expressão emocional.(2,8,14,16)
Educação/informação O MyCyFAPP possui recursos e ferramentas educacionais para a autogestão nutricional personalizada da doença e o empoderamento dos pacientes. Essas ferramentas educacionais são um manual de recomendações nutricionais, repleto de exemplos práticos e recomendações aplicáveis, escritos em linguagem simples e de fácil leitura, incluindo imagens, infográficos e layouts; um jogo para tablets, chamado My Happy Pat, projetado para crianças com FC entre 4 e 11 anos de idade; uma ferramenta projetada especificamente para a criação de receitas com base em bancos de dados de composição nutricional completos e confiáveis, chamada MyFoodCAL; uma ferramenta que aprimora e reformula os bancos de dados de composição nutricional existentes, adicionando novos alimentos e preenchendo lacunas de informações nutricionais, chamada MyFoodFACTS; e uma ferramenta online para compilação de relatos de caso, chamada MyFoodREC.(8,16)
Para pacientes com asma, também existem recursos educacionais disponíveis para ajudar no aprendizado sobre a doença, incluindo sintomas, causas e técnicas eficazes de gestão. O aplicativo Ask Me, AsthMe! fornece recursos educacionais para ajudar os usuários (pacientes e pais) a aprender sobre a asma, seus sintomas e causas e a gerenciar sua condição de forma mais eficaz.(7) O aplicativo ASTHMAXcel contém vídeos educacionais sobre como a asma afeta as vias aéreas, medicamentos e seu funcionamento, monitoramento por fluxômetro e o uso correto de inaladores e espaçadores.(15) Além disso, os aplicativos Kiss my Asthma, Asthma First Aid e Menzies Asthma fornecem instruções educacionais sobre como gerenciar as crises de asma e quando procurar atendimento médico.(13,17,18)
Tratamento farmacológico O aplicativo Genia permite que os pacientes acompanhem a ingestão de medicamentos e compartilhem comentários, ajudando os usuários a manter um registro de quando tomaram sua medicação e qual foi ela, facilitando assim a gestão medicamentosa. (2,14) O MyCyFAPP inclui um plano medicamentoso personalizado para cada usuário individual.(8,16) Esse plano inclui dosagem personalizada por ingestão, recorrência e término da medicação e fornece lembretes para doses médicas. Os usuários também podem acompanhar a adesão aos medicamentos ao longo do tempo utilizando esse recurso.(8,16) Para crianças com asma, os aplicativos Kiss my Asthma e Ask Me, AsthMe! contêm um campo para registro de um diário de medicamentos.(7,13) Isso pode ajudar as crianças a fazer o acompanhamento do cronograma de medicamentos e garantir a adesão ao plano de tratamento prescrito.
Emergência O aplicativo Kiss my Asthma oferece acesso a um plano de ação, instruções de primeiros socorros e contatos de emergência, bem como informações sobre a asma e sobre medicamentos e dispositivos para asma e instruções para a gestão da ansiedade. (13) O aplicativo Ask Me, AsthMe! fornece instruções passo a passo sobre o que fazer em uma situação de emergência. As instruções são organizadas em zonas codificadas por cores, o que torna fácil compreendê-las e segui-las.(7) O aplicativo Asthma First Aid permite que os usuários sigam as etapas de primeiros socorros em tempo real em modo de ataque e revisem as etapas de primeiros socorros utilizando uma amostra de cenários em modo de cenário de treinamento.(17) O aplicativo Menzies Asthma ajuda as crianças a aprender as quatro etapas a seguir em situações de emergência em asma e o que fazer quando os sintomas não melhoram.(18)
Suporte Ao utilizar o aplicativo Genia, os pacientes ou pais podem registrar diariamente observações de saúde e sintomas entre as consultas (atividade física ou problemas gastrointestinais, por exemplo), acompanhar a ingestão de medicamentos e preencher relatórios de pré-consulta, incluindo preferências e metas de tratamento, antes de uma consulta clínica. Essas informações relatadas pelos pacientes permitem que eles documentem a atividade da doença e suas preferências em tempo real entre as consultas clínicas. (2,14) O MyCyFAPP fornece lembretes de medicamentos que ajudam os usuários a lembrar de tomar seus medicamentos na hora certa, lembretes de consultas com PS e acompanhamento do progresso. O aplicativo também inclui um rastreador de sintomas, que permite aos usuários monitorar seus sintomas ao longo do tempo e compartilhar essas informações com os PS, oferecendo flexibilidade para acomodar consultas com recorrências diárias, datas de término ou diferentes dosagens de medicação.(8,16) Para pacientes com asma, o aplicativo Kiss my Asthma fornece a opção de o usuário receber notificações autodefinidas sobre o uso de dispositivos para o controle da asma bem como informações sobre o ambiente de suporte e informações de contato direto. Essa ferramenta pode ajudar as crianças a cumprir os planos de tratamento e monitorar o controle da asma.(13)
Tratamento não farmacológico O aplicativo Genia funciona como um diário de autorrelato, permitindo que crianças com FC registrem e salvem observações sobre diversos aspectos de sua condição.(2,14) Inclui recursos relacionados à função pulmonar, limpeza das vias aéreas, atividade física, apetite e outras terapias de suporte. Elas podem compartilhar seus pensamentos, sentimentos e quaisquer observações que tenham sobre sua rotina terapêutica. Dá-lhes a oportunidade de expressar como percebem a terapia, se a consideram útil ou desafiadora e se têm alguma preocupação ou sugestão a ela relacionada. Ao coletar essas informações por meio do aplicativo Genia, os PS e os cuidadores podem obter insights valiosos sobre a perspectiva da criança e tomar decisões informadas sobre o plano de tratamento. Também empodera as crianças para que participem ativamente dos seus cuidados e se envolvam na gestão da sua condição.(2,14) O MyCyFAPP oferece um plano nutricional personalizado, adaptado às necessidades do indivíduo com base na idade, peso, altura e outros fatores. O plano nutricional fornece informações sobre a ingestão calórica recomendada, o planejamento de refeições e o tamanho das porções e permite que os usuários acompanhem sua ingestão diária de alimentos.(8,16)
DISCUSSÃO Esta revisão teve como objetivo mapear e classificar os estudos existentes sobre aplicativos de mHealth projetados para serem utilizados na autogestão farmacológica e não farmacológica de DPC em crianças e adolescentes.
A implementação de uma abordagem de co-design envolvendo múltiplas partes interessadas é bastante promissora para facilitar a autogestão de DPC.(2,8) Esse processo colaborativo serve dois propósitos principais: em primeiro lugar, ajuda a identificar e abordar divergências entre as partes interessadas, conduzindo assim a soluções eficazes. Em segundo lugar, permite projetar conceitos alinhados com requisitos funcionais (lembretes, notificações, recursos educacionais e suporte, por exemplo) e com aspectos não funcionais como privacidade e economia de tempo. (8) As pesquisas sobre o desenvolvimento da tecnologia de mHealth promovem a incorporação do usuário final ao processo de design; no entanto, as contribuições desses usuários são frequentemente incorporadas tardiamente ou esporadicamente durante a fase de design.(19) Alguns aplicativos desse domínio adotaram com sucesso o co-design para enriquecer seu conteúdo e dar suporte à autogestão da doença. (2,8) O design dos aplicativos é muito importante para que os usuários possam aumentar sua interação e obter mais benefícios com o tratamento terapêutico. No entanto, apenas um aplicativo foi testado em estudos clínicos quanto à sua eficácia no suporte à autogestão da doença.(20)
Os aplicativos de mHealth selecionados nesta revisão de mapeamento abrangem uma série de áreas essenciais, fornecendo conteúdo valioso em cinco domínios principais: educação/informação, tratamento farmacológico, assistência de emergência, suporte e tratamento não farmacológico. Cada um desses componentes oferece benefícios e resultados distintos aos usuários.
O aspecto educação/informação fornece conhecimentos e recursos valiosos para aprimorar a compreensão e a gestão da doença.(7,8,13,15-18) Os módulos de tratamento farmacológico concentram-se no suporte para a adesão aos medicamentos e na otimização dos resultados do tratamento.(2,7,13,14,16) As funcionalidades de assistência emergencial garantem acesso imediato a assistência e recursos durante situações críticas, como uma crise de asma.(7,13,17,18) As ferramentas de tratamento não farmacológico fornecem abordagens e estratégias alternativas para a autogestão da doença.(2,8,14,16) Esses componentes abrangentes contribuem coletivamente para uma experiência de usuário holística e completa com os aplicativos de mHealth selecionados. Por fim, as funcionalidades de suporte oferecem um senso de comunidade e apoio emocional aos indivíduos com a condição.(2,7,13,14,16)
A reavaliação dos aplicativos pelos usuários (crianças, adolescentes, pais e PS) provou ser inestimável para a melhoria da funcionalidade de cada aplicativo. Os usuários expressam um forte desejo de se comunicar com os PS, partilhar informações abrangentes sobre os seus sintomas e receber lembretes sobre a adesão aos medicamentos. As solicitações dos usuários durante a reavaliação dos aplicativos desempenham um papel fundamental na modificação significativa do conteúdo dos aplicativos. Como resultado, funcionalidades como monitoramento de sintomas, terapias sugeridas, medicamentos prescritos e outras atividades relacionadas à terapia diária foram incorporadas para aprimorar a usabilidade e a facilidade de uso. Vale ressaltar que, inicialmente, os aplicativos não contemplavam integralmente essas funcionalidades; no entanto, passaram por melhorias substanciais com a avaliação e o feedback dos usuários.(2,8,14) Curiosamente, ressalta-se que havia limitações nas capacidades de alguns aplicativos de mHealth de reforçar plenamente a autogestão da doença e fornecer informações abrangentes relacionadas à adesão ao tratamento.
No geral, esta revisão destaca o potencial da tecnologia de mHealth no empoderamento de crianças e adolescentes com DPC por meio da autogestão. Os achados reforçam a significância da abordagem de co-design envolvendo todas as partes interessadas relevantes. Ao aproveitar ao máximo os pontos fortes dos aplicativos de mHealth nos domínios de educação, tratamento farmacológico, assistência de emergência, suporte e tratamento não farmacológico, podem-se fornecer suporte à autogestão e comunicação médico-paciente a crianças com DPC e seus familiares, sendo que essa poderosa ferramenta pode aumentar a capacidade desses indivíduos de gerenciar os sintomas da doença e melhorar os resultados de saúde e a qualidade de vida. Mais pesquisas com ensaios controlados randomizados e acompanhamento de longo prazo do uso desses aplicativos em populações pediátricas com FC, asma e bronquiectasia não fibrocística são necessárias para abordar os potenciais benefícios desses aplicativos no suporte a pacientes pediátricos para a gestão de suas condições de forma eficaz.
Esta revisão sistemática de mapeamento apresenta algumas limitações. Embora nossa pesquisa tenha incluído três diferentes bancos de dados, a estratégia de pesquisa foi prejudicada pela exclusão de outros bancos de dados que poderiam ter trazido à luz mais estudos. Nossa pesquisa limitou-se ainda a estudos publicados apenas em inglês, o que pode ter excluído fontes valiosas de informação publicadas em outras línguas. No entanto, acreditamos que há relativamente pouca evidência de pesquisas abordando as questões específicas selecionadas, o que é demonstrado pelo pequeno número de estudos que se enquadraram nos critérios de inclusão bastante específicos desta revisão. Além disso, a heterogeneidade das metodologias e dos contextos nos estudos incluídos apresenta um desafio para a reunião de achados relacionados e contrastantes. Além das limitações supracitadas, vale ressaltar que houve falta de comunicação direta entre nossa equipe de pesquisadores e os autores dos estudos, o que limitou as oportunidades para considerações adicionais e outros possíveis insights. A ausência dessa colaboração pode ter resultado em uma potencial redução da profundidade e da abrangência das informações reunidas nesta revisão.
CONSIDERAÇÕES FINAIS Os aplicativos de mHealth estão se tornando cada vez mais parte da nova era da eHealth. Essas ferramentas contam com diversos recursos e funções, tendo como objetivo dar suporte aos usuários e melhorar a adesão ao tratamento e, consequentemente, melhorar a autogestão da doença. Tendo com foco especificamente aplicativos para crianças/adolescentes, os aplicativos de mHealth são projetados com uma abordagem voltada para o usuário, levando em consideração o feedback de pacientes, pais/cuidadores e PS. Esse esforço colaborativo tem como objetivo aprimorar a funcionalidade dos aplicativos, garantindo que eles atendam às necessidades e preferências específicas dos usuários pretendidos. Esta revisão de mapeamento identificou cinco áreas de conteúdo nos aplicativos de mHealth para crianças com DPC: educação/informação, tratamento farmacológico, emergência, suporte e tratamento não farmacológico. O desafio para os PS reside na seleção do produto final melhorado. Para garantir a usabilidade e eficácia na obtenção de resultados clínicos como a promoção da adesão a tratamentos farmacológicos e não farmacológicos e a melhoria da qualidade de vida são necessários mais estudos clínicos envolvendo esses pacientes. Esses estudos fornecerão insights valiosos sobre o impacto e a eficácia dos aplicativos, contribuindo, em última análise, para o seu contínuo desenvolvimento e aperfeiçoamento.
AGRADECIMENTOS Os autores gostariam de agradecer ao Sr. Nicholas Nikolovienis a edição do manuscrito final.
CONTRIBUIÇÕES DOS AUTORES VS e EK: concepção e delineamento do estudo; redação inicial do manuscrito; revisão crítica do conteúdo intelectual; redação da versão final do manuscrito. VS, PK, EP, TM e PD: análise e interpretação dos dados. Todos os autores aprovaram a versão final do manuscrito.
CONFLITOS DE INTERESSE Nenhum declarado.
REFERÊNCIAS 1. Catarino M, Charepe Z, Festas C. Promotion of Self-Management of Chronic Disease in Children and Teenagers: Scoping Review. Healthcare (Basel). 2021;9(12):1642. https://doi.org/10.3390/healthcare9121642
2. Longacre M, Grande S, Hager A, Montan M, Bergquist RP, Martensson M, et al. Clinical Adoption of mHealth Technology to Support Pediatric Cystic Fibrosis Care in Sweden: Qualitative Case Study. JMIR Pediatr Parent. 2018;1(2):e11080. https://doi.org/10.2196/11080
3. Licari A, Ferrante G, Marseglia Md GL, Corsello Md G, La Grutta S. What Is the Impact of Innovative Electronic Health Interventions in Improving Treatment Adherence in Asthma? The Pediatric Perspective. J Allergy Clin Immunol Pract. 2019;7(8):2574-2579. https://doi.org/10.1016/j.jaip.2019.08.008
4. Mascheroni G, Ólafsson K. The mobile Internet: Access, use, opportunities and divides among European children. New Media Soc. 2016;18(8):1657-1679. https://doi.org/10.1177/1461444814567986
5. Kosse RC, Bouvy ML, de Vries TW, Kaptein AA, Geers HC, van Dijk L, et al. mHealth intervention to support asthma self-management in adolescents: the ADAPT study. Patient Prefer Adherence. 2017;11:571-577. https://doi.org/10.2147/PPA.S124615
6. Farzandipour M, Nabovati E, Sharif R, Arani MH, Anvari S. Patient Self-Management of Asthma Using Mobile Health Applications: A Systematic Review of the Functionalities and Effects. Appl Clin Inform. 2017;8(4):1068-1081. https://doi.org/10.4338/ACI-2017-07-R-0116
7. Franzmair J, Diesner-Treiber SC, Voitl JJM, Voitl P. Effective German and English Language mHealth Apps for Self-management of Bronchial Asthma in Children and Adolescents: Comparison Study. JMIR Mhealth Uhealth. 2021;9(5):e24907. https://doi.org/10.2196/24907
8. Vilarinho T, Floch J, Stav E. Co-designing a mHealth Application for Self-management of Cystic Fibrosis. Proceedings of the 16th 16th IFIP TC 13 International Conference Part III; 2017 Sep 25-29; Mumbai, India. New York: Springer. FIP Conference on Human-Computer Interaction (INTER-ACT). Sep 2017, Mumbai, India. p.3-22. https://doi.org/10.1007/978-3-319-67687-6_1
9. Klok T, Kaptein AA, Brand PLP. Non-adherence in children with asthma reviewed: The need for improvement of asthma care and medical education. Pediatr Allergy Immunol. 2015;26(3):197-205. https://doi.org/10.1111/pai.12362
10. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91-108. https://doi.org/10.1111/j.1471-1842.2009.00848.x
11. Social Care Institute for Excellence (SCIE) [homepage on the Internet]. Egham, UK: SCIE [updated 2009]. Clapton J, Rutter D, Shariff N. SCIE Systematic mapping guidance. Available from: https://www.scie.org.uk/almost-there
12. Fernández-Sotos P, Torio I, Fernández-Caballero A, Navarro E, González P, Dompablo M, et al. Social cognition remediation interventions: A systematic mapping review. PLoS One. 2019;14(6):e0218720. https://doi.org/10.1371/journal.pone.0218720
13. Davis SR, Peters D, Cavo RA, Sawyer SM, Foster JM, Smith L. “Kiss myAsthma”: Using a participatory design approach to develop a self-management app with young people with asthma. J Asthma. 2018;55(9):1018-1027. https://doi.org/10.1080/02770903.2017.1388391
14. Rutland SB, Bergquist RP, Hager A, Geurs R, Mims C, Gutierrez HH, et al. A Mobile Health Platform for Self-Management of Pediatric Cystic Fibrosis: Qualitative Study of Adaptation to Stakeholder Needs and Integration in Clinical Settings. JMIR Form Res. 2021;5(1):e19413. https://doi.org/10.2196/19413
15. Hsia BC, Singh AK, Njeze O, Cosar E, Mowrey WB, Feldman J, et al. Developing and evaluating ASTHMAXcel adventures: A novel gamified mobile application for pediatric patients with asthma. Ann Allergy Asthma Immunol. 2020;125(5):581-588. https://doi.org/10.1016/j.anai.2020.07.018
16. Calvo-Lerma J, Martinez-Jimenez CP, Lázaro-Ramos JP, Andrés A, Crespo-Escobar P, Stav E, et al. Innovative approach for self-management and social welfare of children with cystic fibrosis in Europe: development, validation and implementation of an mHealth tool (MyCyFAPP). BMJ Open. 2017;7(3):e014931. https://doi.org/10.1136/bmjopen-2016-014931
17. Bajis D, Chaar B, Basheti I, Moles R. Teaching asthma first aid to pharmacy students: A comparative study between an online course and simulation by role-play. Pharm Educ. 2021; 21(1):92-104. https://doi.org/10.46542/pe.2021.211.92104
18. Versteegh LA, Chang AB, Chirgwin S, Tenorio FP, Wilson CA, McCallum GB. Multi-lingual “Asthma APP” improves health knowledge of asthma among Australian First Nations carers of children with asthma. Front Pediatr. 2022;10:925189. https://doi.org/10.3389/fped.2022.925189
19. Harte R, Glynn L, Rodriguez-Molinero A, Baker PM, Scharf T, Quinlan LR, et al. A Human-Centered Design Methodology to Enhance the Usability, Human Factors, and User Experience of Connected Health Systems: A Three-Phase Methodology. JMIR Hum Factors. 2017;4(1):e8. https://doi.org/10.2196/humanfactors.5443
20. Calvo-Lerma J, Boon M, Hulst J, Colombo C, Asseiceira I, Garriga M, et al. Change in Nutrient and Dietary Intake in European Children with Cystic Fibrosis after a 6-Month Intervention with a Self-Management mHealth Tool. Nutrients. 2021;13(6):1801. https://doi.org/10.3390/nu13061801