ABSTRACT
Objective: To compare somatic growth, lung function, and level of physical activity in schoolchildren who had been very-low-birth-weight preterm infants (VLBWPIs) or normal-birth-weight full-term infants. Methods: We recruited two groups of schoolchildren between 8 and 11 years of age residing in the study catchment area: those who had been VLBWPIs (birth weight < 1,500 g); and those who had been normal-birth-weight full-term infants (controls, birth weight ≥ 2,500 g). Anthropometric and spirometric data were collected from the schoolchildren, who also completed a questionnaire regarding their physical activity. In addition, data regarding the perinatal and neonatal period were collected from the medical records of the VLBWPIs. Results: Of the 93 schoolchildren screened, 48 and 45 were in the VLBWPI and control groups, respectively. No significant differences were found between the groups regarding anthropometric characteristics, nutritional status, or pulmonary function. No associations were found between perinatal/neonatal variables and lung function parameters in the VLBWPI group. Although the difference was not significant, the level of physical activity was slightly higher in the VLBWPI group than in the control group. Conclusions: Among the schoolchildren evaluated here, neither growth nor lung function appear to have been affected by prematurity birth weight, or level of physical activity.
Keywords:
Premature birth; Birth weight; Respiratory function tests; Motor activity; Pediatrics.
RESUMO
Objetivo: Comparar o crescimento somático, a função pulmonar e o nível de atividade física entre escolares nascidos prematuros com muito baixo peso e escolares nascidos a termo e com peso adequado. Métodos: Foram recrutados escolares com idade de 8 a 11 anos residentes na mesma área de abrangência do estudo: prematuros e com peso < 1.500 g e controles (nascidos a termo e com peso ≥ 2.500 g). Foram obtidas medidas antropométricas e espirométricas e aplicado um questionário sobre a atividade física. Além disso, foram coletadas informações do período perinatal/neonatal dos recém-nascidos com muito baixo peso (RNMBP) de seus prontuários médicos. Resultados: Dos 93 escolares avaliados, 48 crianças no grupo RNMBP e 45 no grupo controle. Não houve diferenças significativas entre os grupos em relação às características antropométricas e nutricionais ou aos parâmetros de função pulmonar. Não foram encontradas associações entre as variáveis perinatais/neonatais e parâmetros da função pulmonar dos escolares no grupo RNMBP. Embora sem diferença significativa em relação aos níveis de atividade física, o grupo RNMBP apresentou uma tendência de ser mais ativo que o grupo controle. Conclusões: Nos escolares aqui estudados o crescimento e a função pulmonar parecem não ser afetados por prematuridade, peso ao nascimento ou nível de atividade física.
Palavras-chave:
Nascimento prematuro; Peso ao nascer; Testes de função respiratória; Atividade motora; Pediatria.
INTRODUÇÃOTerapias com surfactante e uso de esteroides pré-natais fizeram com que os recém-nascidos com muito baixo peso (RNMBP) obtivessem uma notável redução de mortalidade.(1) Apesar disso, os longos períodos de suplementação de oxigênio ou de ventilação mecânica que muitos prematuros necessitam podem colaborar para danos irreversíveis do parênquima pulmonar.(2)
Embora vários estudos tenham avaliado os efeitos da prematuridade, do baixo peso ao nascimento e de algumas características do período neonatal sobre a função pulmonar ao longo da infância, ainda persistem achados contradi-tórios sobre esses aspectos ao longo da idade escolar nesses indivíduos. Enquanto alguns estudos mostraram uma redução de VEF1, CVF e volumes pulmonares em prematuros,(3,4) outros evidenciaram uma preservação da condição pulmonar na infância.(5,6) Além disso, até o presente momento, não foram localizados estudos realizados no Brasil que tenham avaliado a evolução da função pulmonar de RNMBP em idade escolar.
Em crianças nascidas pré-termo, parte do desenvolvimento pulmonar acontece após o nascimento, o que prejudica o processo natural de desenvolvimento pulmonar e das vias aéreas.(7) Os padrões de remodelamento em um siste-ma respiratório imaturo ocorrem de acordo com o estágio de desenvolvimento afetado.(8) Estudos prévios relataram que os fatores neonatais e perinatais parecem ser capazes de desencadear uma sequência de eventos que podem comprometer as estruturas pulmonares e causar um aumento da incidência de doenças respiratórias.(7,9)
Crianças nascidas prematuras e aquelas com extremo baixo peso podem apresentar um risco aumentado de de-senvolver complicações de saúde e atraso no desenvolvimento quando comparadas àquelas nascidas a termo na idade escolar.(10) Além disso, estudos sugerem que crianças prematuras apresentam recuperação lenta e tardia do crescimento, com alto risco de crescimento inadequado nos primeiros anos de vida,(11,12) e que a deficiência pônde-ro-estatural observada nos primeiros meses de vida pode persistir por toda a infância, adolescência e idade adul-ta.(13)
Nas duas últimas décadas também vêm ocorrendo uma redução expressiva do nível de atividade física e um au-mento do comportamento sedentário na faixa etária pediátrica.(14,15) Essas alterações podem ser atribuídas às mu-danças no perfil das atividades realizadas pelos jovens, substituindo atividades ativas e com maior gasto energético por horas em frente ao computador, ao videogame e à televisão.(14) No entanto, ainda são limitadas as informações sobre os níveis de atividade física em escolares que nasceram prematuros e/ou com baixo peso ao nascimento.(16,17)
Portanto, os achados contraditórios da função pulmonar em crianças que nasceram prematuras e com baixo peso em idade escolar, e o possível comprometimento do crescimento pôndero-estatural desses indivíduos, com mudan-ças importantes no perfil das atividades físicas, são as questões que motivaram o desenvolvimento do presente estudo. Os objetivos específicos do estudo foram os de avaliar o crescimento, a função pulmonar e o nível de ativi-dade física em escolares entre 8 e 11 anos de idade, nascidos prematuros com muito baixo peso, e compará-los com escolares da mesma faixa etária nascidos a termo e com peso adequado.
MÉTODOSTrata-se de um estudo caso-controle. Foram incluídas crianças que nasceram prematuras e com peso ≤ 1.500 g que estiveram internadas na UTI Neonatal do Hospital Geral de Caxias do Sul, em Caxias do Sul (RS), entre janeiro de 2001 e dezembro de 2005 e que tinham idade entre 8 e 11 anos no momento do estudo. Por razões de logística, foram convidadas crianças que residiam em municípios até 100 km de distância de Caxias do Sul. Os sujeitos foram convidados para participar do estudo via contato telefônico.
O grupo controle foi composto por crianças nascidas a termo (≥ 37 semanas de idade gestacional), com peso de nascimento ≥ 2.500 g, com ausência de sintomas respiratórios baseados no questionário do International Study of Asthma and Allergies in Children(18) e recrutadas em escolas públicas de Caxias do Sul. Foram excluídos, em ambos os grupos, indivíduos que apresentavam doença cardíaca, doença neuromuscular, limitações cognitivas ou incapaci-dade de realizar o teste de espirometria.
A coleta de dados foi realizada na Universidade de Caxias do Sul, por dois pesquisadores treinados, no período entre julho e dezembro de 2013. O estudo foi aprovado pelo Comitê de Ética e Pesquisa da Pontifícia Universidade Católica do Rio Grande do Sul, em Porto Alegre (RS), sob o número 12323413.7.0000.5336, e os familiares leram e assinaram o termo de consentimento livre e esclarecido, com o assentimento das crianças.
As informações sobre o período perinatal e neonatal do grupo de RNMBP foram extraídas do banco de dados da UTI neonatal. Foram coletadas as seguintes variáveis: uso de corticoide antenatal, ruptura prematura das membra-nas, tempo de oxigenoterapia, tempo de internação, peso ao nascimento, uso de pressão positiva contínua em vias aéreas, doença da membrana hialina e uso de surfactante.
O peso foi mensurado com uma balança digital (Glass 1 FW; G-Tech, Rio de Janeiro, Brasil), e a altura, por meio de um estadiômetro portátil (Alturaexata; TBW, São Paulo, Brasil). A partir dessas aferições, as características nutricio-nais foram normalizadas através do escore Z para os indicadores altura, peso e IMC corrigidos pela idade.(19)
A espirometria foi realizada com um espirômetro portátil (Koko; Ferraris Respiratory, Louisville, CO, EUA). Segui-mos os procedimentos e os critérios de aceitabilidade e reprodutibilidade da American Thoracic Society.(20) As crian-ças foram verbalmente encorajadas a exalar o volume máximo de ar, a partir de uma inspiração máxima, com má-ximo esforço.(20) Os parâmetros espirométricos avaliados incluíram CVF, VEF1 e FEF25-75%. Os resultados foram expres-sos em valores absolutos e normalizados através do escore Z.(21)
A avaliação do nível de atividade física foi realizada utilizando-se um questionário adaptado, composto por ques-tões referentes às atividades desenvolvidas nos últimos sete dias.(14) Esse instrumento incluiu informações sobre modo, tempo de deslocamento para a escola e/ou trabalho e a frequência/tempo despendido para cada atividade física no lazer. Os escolares foram classificados, de acordo com o nível de atividade física, em ativos (> 300 min/semana) e inativos (≤ 300 min/semana); os considerados com comportamento sedentário foram diferenciados em relação ao tempo diário em frente a uma tela (> 2 h/dia ou ≤ 2 h/dia).(22)
O tamanho amostral de 25 indivíduos para cada grupo foi suficiente para detectar uma diferença de 14% no FEV1 em porcentagem do predito, assumindo-se um desvio-padrão de 12% no grupo controle e de 17% no grupo RNMBP (com base em um estudo prévio, com um poder de 90% e um nível de significância de 5%).(23) Esse número foi acrescido para 30 em cada grupo, totalizando 60 pacientes, considerando-se as possíveis perdas no estudo.
As variáveis do estudo foram avaliadas através do teste de Kolmogorov-Smirnov. Os dados que apresentaram dis-tribuição normal foram apresentados em média e desvio-padrão, enquanto as variáveis assimétricas, em mediana e intervalo interquartil. Os dados categóricos foram apresentados em frequência absoluta e relativa. A comparação dos desfechos avaliados entre os dois grupos foi realizada através do teste t de Student para amostras independentes, teste U de Wilcoxon e teste de qui-quadrado de Pearson. Para a avaliação da associação entre as variáveis de desfe-cho (VEF1, CVF e FEF25-75%) e as variáveis preditoras (peso ao nascimento, dias de internação, idade gestacional, ruptura prematura das membranas, uso de surfactante, uso de corticoide antenatal, dias de oxigenoterapia, tempo de ventilação mecânica, uso de pressão positiva contínua nas vias aéreas e doença da membrana hialina), utilizaram-se modelos de regressão linear univariada e multivariada. Todas as análises foram realizadas no programa Statisti-cal Package for the Social Sciences, versão 18.0 (SPSS Inc., Chicago, IL, EUA), e as diferenças foram consideradas significativas quando p < 0,05.
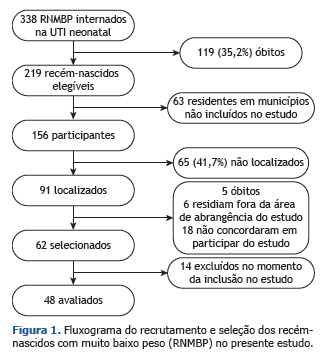
RESULTADOSDe um total de 338 RNMBP internados na UTI neonatal durante o período selecionado para a coleta de dados, 219 (64,79%) sobreviveram. Desses, 91 (41,55%) foram localizados, e apenas 62 (28,31%) foram selecionados para participar do estudo. A Figura 1 demonstra os dados referentes à seleção do grupo RNMBP.
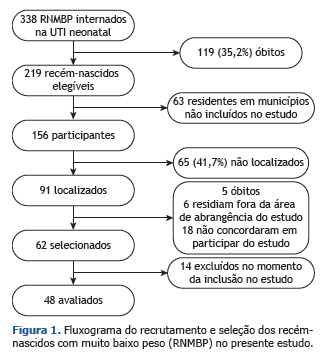
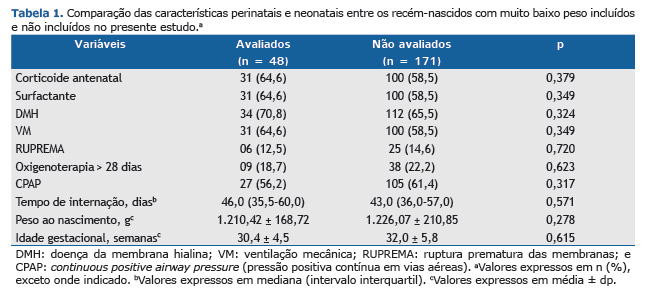
A partir dos 62 RNMBP selecionados, 7 foram excluídos por realizarem testes espirométricos inadequados tecnica-mente, e 7, por apresentarem déficit cognitivo incompatível com o exame. Assim, foi selecionado um total de 48 (77,41%) participantes. A Tabela 1 apresenta as informações do período perinatal e neonatal desses participantes no grupo RNMBP. Não houve diferenças significativas na comparação das características do período neonatal e perinatal entre os indivíduos incluídos e não incluídos no grupo RNMBP no presente estudo.
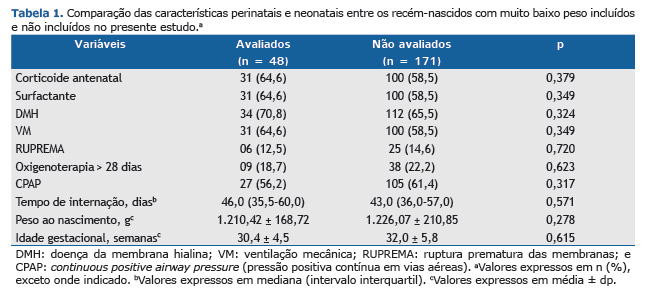
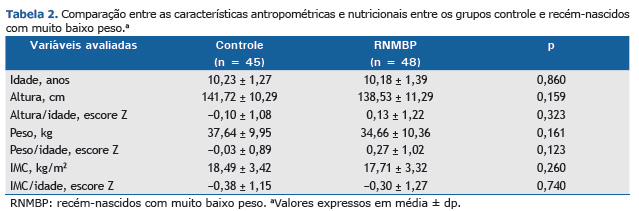
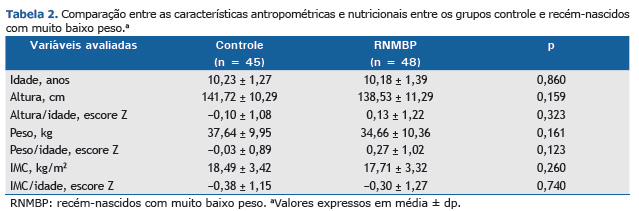
Em paralelo a esse grupo, foram selecionados 52 controles. Desses, 5 foram excluídos por insucesso na espirome-tria, e 2, por déficit cognitivo, resultando em um total de 45 controles (86,53%). Assim, a amostra final do presente estudo foi composta por um total de 93 crianças, sendo 48 do grupo RNMBP e 45 no grupo controle. Não houve dife-renças significativas em relação às características antropométricas e nutricionais entre os dois grupos avaliados (Tabela 2).
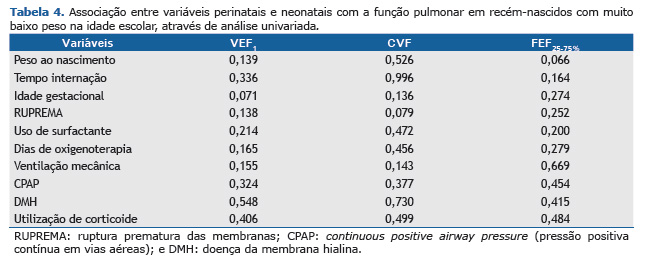
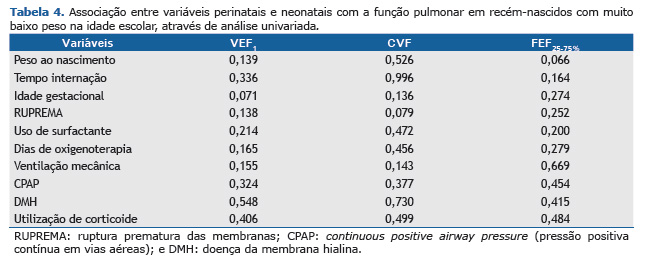
Em relação aos dados da função pulmonar, não houve diferenças significativas na comparação das médias das va-riáveis espirométricas entre os grupos controle e RNMBP (Tabela 3). Grande parte da amostra estudada apresentou valores espirométricos normais, isto é, escore Z acima de −1,645 nas variáveis analisadas. Seis participantes do grupo RNMBP apresentaram redução no VEF1. Esses, quando comparados aos outros 42 participantes do grupo RNMBP, apresentaram valores significativamente menores nas médias de idade gestacional (28,1 ± 0,9 semanas; p = 0,006) e de peso ao nascimento (1.015,0 ± 122,7 g; p = 0,008). Embora se perceba diferenças também quanto aos dados do número de dias de internação hospitalar [mediana = 54,0 (42,0-66,0); p = 0,249] e da necessidade de oxigenoterapia por mais de 28 dias [n = 3 (60%); p = 0,083] não houve diferenças significativas. As características perinatais e neonatais não implicaram em associações significativas com dados da função pulmonar na idade escolar nas análises de regressão linear univariada e multivariada. A Tabela 4 demonstra as associações estudadas por meio da análise univariada.

Em relação à classificação dos níveis de atividade física, 34 (36,5%) dos participantes avaliados foram considera-dos ativos, enquanto 59 (63,4%) foram classificados como inativos. Houve uma tendência de os participantes do grupo RNMBP ser mais ativos do que os do grupo controle; todavia, não houve diferença significativa (p = 0,055) sobre esse desfecho (Figura 2A). Nos grupos RNMBP e controle, as atividades físicas mais comuns no lazer foram futebol (37,5% vs. 22,2%; p = 0,108), seguidas de corrida (27,9% vs. 22,2%; p = 0,936) e bicicleta (14,6% vs. 31,1%; p = 0,057). O tempo médio despendido com deslocamento ativo foi de 20,55 ± 5,89 min e 19,75 ± 6,78 min (p = 0,737) nesses grupos, respectivamente. Por fim, embora 90 (96,7%) dos participantes avaliados tenham perma-necido mais de 2 h/dia em frente a uma tela, não houve uma diferença significativa (p = 0,596) na comparação entre os dois grupos avaliados (Figura 2B).
 DISCUSSÃO
DISCUSSÃOOs achados do presente estudo demonstraram resultados similares de crescimento pôndero-estatural e de função pulmonar, assim como uma tendência de o grupo RNMBP ser mais ativo em comparação aos indivíduos controles.
Estudos prévios, que avaliaram o crescimento de RNMBP desde a alta até o início da vida adulta, ressaltaram a importância desse acompanhamento na identificação de deficiências de crescimento e suas consequências.(11,12) Alguns desses estudos relataram que o fato de as crianças nascer com baixo peso constituiu-se um fator de risco para déficits no crescimento e no IMC.(11,24) Por outro lado, há um relato de que fatores genéticos e condições socioe-conômicas têm uma maior influência sobre o crescimento nessas crianças, na idade escolar, do que o baixo peso ao nascimento.(25) Esses achados estão em acordo com os descritos no presente estudo, no qual se verificou que os escolares nascidos com muito baixo peso apresentavam características antropométricas e nutricionais similares às do grupo controle.
Embora o desenvolvimento do sistema respiratório possa encontrar-se alterado devido à prematuridade e às inter-venções que dela decorrem,(9) os resultados do presente estudo não evidenciaram redução da função pulmonar nos escolares do grupo RNMBP em comparação aos controles nascidos a termo, quando avaliados quase uma década após o nascimento. Esses resultados encontram-se de acordo com alguns estudos prévios, nos quais foram identifi-cados achados de função pulmonar preservada(5,6) em escolares e adultos que nasceram prematuros e com baixo peso. Uma das hipóteses mais coerentes para tal resultado é o fato de que as alterações pulmonares podem ser mais aparentes nos primeiros anos de vida e menos evidentes no decorrer da infância, devido aos cuidados dos pais em relação à saúde respiratória, realizando acompanhamento pulmonar periódico e estando alerta a qualquer mudança no quadro respiratório da criança.(7) Além disso, o incentivo para a prática de atividades físicas, associado com um aporte nutricional adequado, pode colaborar na recuperação funcional desses sujeitos.(7) Apesar de alguns estudos sugerirem que os aspectos socioeconômicos e étnicos possam influenciar a função pulmonar desses participan-tes,(26,27) o presente estudo não avaliou a influência desses aspectos na amostra estudada.
Os resultados de função pulmonar preservada obtidos em nossa amostra diferem-se de outros dados anteriores, que demonstraram um comprometimento da condição pulmonar nesse grupo de pacientes em idade escolar.(3,28,29) Um estudo recente relatou também que o risco de comprometimento pulmonar é ainda maior na idade escolar em prematuros nascidos com menos de 32 semanas e que não receberam terapia com surfactante.(30) Tais divergências quanto aos resultados desses estudos podem ser atribuídas, pelo menos em parte, aos diferentes delineamentos, métodos de avaliação pulmonar, equações de referência utilizadas, definições de prematuridade e classificações de baixo peso ao nascimento.(3,6,31) Apenas 6 escolares do grupo RNMBP apresentaram redução da função pulmonar no momento da avaliação por espirometria. Esse resultado pode ser justificado devido à maior gravidade clínica desses participantes ao nascimento, já que apresentaram uma menor idade gestacional (< 32 semanas) e peso ao nasci-mento (< 1.200 g), além de permanecer mais dias internados e com suplementação de oxigênio, quando compara-dos aos demais participantes do grupo RNMBP.
Os achados do presente estudo não evidenciaram associações das variáveis perinatais e neonatais com a função pulmonar em idade escolar. Esse resultado está em acordo com o de um estudo recente, o qual demonstrou que nenhum fator perinatal foi significativamente relacionado com as variáveis de função respiratória.(32) Além disso, nosso resultado é similar ao de outro estudo, no qual o baixo peso ao nascimento e a idade gestacional não estavam relacionados com a redução da função pulmonar em idade escolar.(31) Em contrapartida, outros estudos demonstra-ram a influência desses fatores, como o tempo de oxigenoterapia e dias de ventilação mecânica, em crianças nasci-das prematuras e com muito baixo peso.(9,33) Apesar de o grupo RNMBP avaliado ter sido exposto, nos primeiros dias de vida, a diversos agentes, como oxigenoterapia e/ou ventilação mecânica, um estudo anterior relatou que qual-quer anormalidade da função pulmonar de crianças em idade escolar que foram expostas a esses fatores pode estar mais relacionada à prematuridade do que à própria lesão pulmonar neonatal.(34) Estudos prévios realizados no nosso laboratório evidenciaram reduções nos fluxos expiratórios máximos em prematuros(35) e que essa anormalidade persistia até o segundo ano de vida.(36) No presente estudo, o grupo RNMBP não apresentou redução na função pul-monar. De acordo com nossos dados, a função pulmonar parece encontrar-se reduzida até o segundo ano de vida, possivelmente normalizando ao longo da idade escolar, paralelamente à redução da morbidade respiratória.
A avaliação dos níveis de atividade física através de questionários de autorrelato é uma alternativa viável e práti-ca para a quantificação do sedentarismo na população jovem,(14) considerando-se os custos elevados de equipamen-tos de avaliação objetiva, como pedômetros e acelerômetros. No presente estudo, utilizou-se um questionário pro-posto por Hallal et al.,(14) através do qual o tempo despendido no deslocamento de casa à escola e/ou trabalho, bem como nas atividades realizadas no lazer, é quantificado. Embora esse instrumento venha sendo amplamente utiliza-do na população pediátrica e pareceu apresentar bom entendimento por parte desta,(14,37) essa ferramenta não quan-tifica o tempo gasto em atividades de acordo com a intensidade do exercício praticado, o que poderia limitar maior conhecimento e interpretação sobre o comportamento físico desses sujeitos.
Os resultados do presente estudo também demonstraram que mais de 60% da amostra estudada foi classificada como inativa, o que, de acordo com estudos brasileiros prévios,(14,37) caracteriza o sedentarismo, um importante problema de saúde pública. Não se encontrou uma diferença significativa nos níveis de atividade física entre os dois grupos avaliados, corroborando os dados de outro estudo comparando crianças nascidas prematuras e controles nascidos a termo.(38) Embora não tenha havido uma diferença significativa, o grupo RNMBP apresentou uma tendên-cia de ser mais ativo quando comparado ao grupo controle. Esse fato pode ser atribuído a fatores familiares, como as preferências dos pais em relação às diferentes atividades físicas, estimulando os filhos à prática dessas atividades, ou à superproteção dos pais em relação a seus filhos. (38) No entanto, a influência desses aspectos não foi avaliada no presente estudo. Mais de 90% das crianças avaliadas em ambos os grupos permaneciam mais de 2 h em frente a uma tela de televisão, videogame ou computador. Tal resultado parece confirmar os achados de estudos nacionais e internacionais,(39,40) os quais demonstraram elevados índices de comportamento sedentário na faixa etária pediátri-ca. Assim, ressalta-se a necessidade da elaboração de medidas estratégicas de combate ao sedentarismo, pois esse, nessa faixa etária, é um fator de risco para a inatividade física na idade adulta.(39)
A principal limitação do presente estudo constitui-se no fato de que a amostra de RNMBP avaliada correspondeu a menos da metade do total de sujeitos disponíveis para recrutamento. Grande parte dessas crianças não foi localiza-da, não residia em municípios incluídos no estudo, não concordou em participar da pesquisa ou foi a óbito. No entan-to, acredita-se que essa limitação não tenha influenciado os resultados obtidos, tendo em vista que foram encontra-dos achados similares em relação às características perinatais e neonatais entre os RNMBP avaliados e não avalia-dos no estudo.
Em conclusão, os resultados do presente estudo demonstraram achados de crescimento pôndero-estatural e de função pulmonar preservados e uma tendência do grupo RNMBP em ser mais ativos em comparação aos sujeitos controles. Além disso, as variáveis do período perinatal e neonatal não foram associadas com a função pulmonar na idade escolar no grupo estudado.
REFERÊNCIAS1. Draper ES, Zeitlin J, Fenton AC, Weber T, Gerrits J, Martens G, et al. Investigating the variations in survival rates for very preterm infants in 10 European regions: the MOSAIC birth cohort. Arch Dis Child Fetal Neonatal Ed. 2009;94(3):F158-63. http://dx.doi.org/10.1136/adc.2008.141531
2. Eber E, Zach MS. Long term sequelae of bronchopulmonary dysplasia (chronic lung disease of infancy). Thorax. 2001;56(4):317-23. http://dx.doi.org/10.1136/thorax.56.4.317
3. Palta M, Sadek-Badawi M, Madden K, Green C. Pulmonary testing using peak flow meters of very low birth weight children born in the perisurfactant era and school controls at age 10 years. Pediatr Pulmonol. 2007;42(9):819-28. http://dx.doi.org/10.1002/ppul.20662
4. Siltanen M, Savilahti E, Pohjavuori M, Kajosaari M. Respiratory symptoms and lung function in relation to atopy in children born preterm. Pediatr Pulmonol. 2004;37(1):43-9. http://dx.doi.org/10.1002/ppul.10402
5. Qi-Qiang H, Tze-Wai W, Lin D, Zhuo-Qin J, Yang G, Guo-Zhen L, et al. Birth weight and lung function in a cohort of Chinese school children. Pediatr Pulmonol. 2009;44(7):662-8. http://dx.doi.org/10.1002/ppul.21035
6. Kitchen WH, Olinsky A, Doyle LW, Ford GW, Murton LJ, Slonim L, et al. Respiratory health and lung function in 8-year-old children of very low birth weight: a cohort study. Pediatrics. 1992;89(6 Pt 2):1151-8.
7. Hjalmarson O, Sandberg K. Abnormal lung function in healthy preterm infants. Am J Respir Crit Care Med. 2002;165(1):83-7. http://dx.doi.org/10.1164/ajrccm.165.1.2107093
8. Stick S. Pediatric origins of adult lung disease. 1. The contribution of airway development to paediatric and adult lung disease. Thorax. 2000;55(7):587-94. http://dx.doi.org/10.1136/thorax.55.7.587
9. Maritz GS, Morley CJ, Harding R. Early developmental origins of impaired lung structure and function. Early Hum Dev. 2005;81(9):763-71. http://dx.doi.org/10.1016/j.earlhumdev.2005.07.002
10. Goyen TA, Lui K. Developmental coordination disorder in "apparently normal" schoolchildren born extremely preterm. Arch Dis Child. 2009;94(4):298-302. http://dx.doi.org/10.1136/adc.2007.134692
11. Hack M, Weissman B, Borawski-Clark E. Catch-up growth during childhood among very low-birth-weight children. Arch Pediatr Adolesc Med. 1996;150(11):1122-9. http://dx.doi.org/10.1001/archpedi.1996.02170360012002
12. Peralta-Carcelen M, Jackson DS, Goran MI, Royal SA, Mayo MS, Nelson KG. Growth of adolescents who were born at extremely low birth weight without major disability. J Pediatr. 2000;136(5):633-40. http://dx.doi.org/10.1067/mpd.2000.104291
13. Cardoso-Demartini AdeA, Bagatin AC, Silva RP, Boguszewski MC. Growth of preterm-born children [Article in Portuguese]. Arq Bras Endocrinol Metabol. 2011;55(8):534-40.
14. Hallal PC, Bertoldi AD, Gonçalves H, Victora CG. Prevalence of sedentary lifestyle and associated factors in adolescents 10 to 12 years of age [Article in Portuguese]. Cad Saude Publica. 2006;22(6):1277-87. http://dx.doi.org/10.1590/S0102-311X2006000600017
15. Fonseca Vde M, Sichieri R, da Veiga GV. Factors associated with obesity among adolescents [Article in Portuguese]. Rev Saude Publica. 1998;32(6):541-9.
16. van Deutekom AW, Chinapaw MJ, Vrijkotte TG, Gemke RJ. Study protocol: the relation of birth weight and infant growth trajectories with physical fitness, physical activity and sedentary behavior at 8-9 years of age - the ABCD study. BMC Pediatr. 2013;13:102. http://dx.doi.org/10.1186/1471-2431-13-102
17. Pianosi PT, Fisk M. Cardiopulmonary exercise performance in prematurely born children. Pediatr Res. 2000;47(5):653-8. http://dx.doi.org/10.1203/00006450-200005000-00016
18. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: ISAAC. The International Study of Asthma and Allergies in Childhood (ISAAC) Steering Committee. Lancet. 1998;351(9111):1225-32. http://dx.doi.org/10.1016/S0140-6736(97)07302-9
19. de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. J Nutr. 2007;137(1):144-8.
20. Miller M, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of Spirometry. Eur Resp J. 2005;26(2):319-38. http://dx.doi.org/10.1183/09031936.05.00034805
21. Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324-43. http://dx.doi.org/10.1183/09031936.00080312
22. Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305(23):2448-55. http://dx.doi.org/10.1001/jama.2011.812
23. Gross SJ, Iannuzzi DM, Kveselis DA, Anbar RD. Effect of preterm birth on pulmonary function at school age: a prospective controlled study. J Pediatr. 1998;133(2):188-92. http://dx.doi.org/10.1016/S0022-3476(98)70219-7
24. Méio MD, Soares FV, Fonseca VM, Villela LD, Boechat MC, Moreira ME. Short stature in 4 to 8 years-old infants with very low birth weight [Article in Portuguese]. Rev Pesq Saude. 2010;11(3):41-5.
25. de Jesus Machado Amorim R, de Carvalho Lima M, Cabral de Lira PI, Emond AM. Does low birthweight influence the nutritional status of children at school age? A cohort study in northeast Brazil. Matern Child Nutr. 2011;7(3):295-306. http://dx.doi.org/10.1111/j.1740-8709.2009.00233.x
26. Yüksel B, Greenough A. Ethnic origin and lung function of infants born prematurely. Thorax. 1995;50(7):773-6. http://dx.doi.org/10.1136/thx.50.7.773
27. Stocks J, Henschen M, Hoo AF, Costeloe K, Dezateux C. Influence of ethnicity and gender on airway function in preterm infants. Am J Respir Crit Care Med. 1997;156(6):1855-62. http://dx.doi.org/10.1164/ajrccm.156.6.9607056
28. Doyle LW; Victorian Infant Collaborative Study Group. Respiratory function at age 8-9 years in extremely low birthweight/very preterm children born in Victoria in 1991-1992. Pediatr Pulmonol. 2006;41(6):570-6. http://dx.doi.org/10.1002/ppul.20412
29. Ronkainen E, Dunder T, Peltoniemi O, Kaukola T, Marttila R, Hallman M. New BPD predicts lung function at school age: Follow-up study and meta-analysis. Pediatr Pulmonol. 2015;50(11):1090-8. http://dx.doi.org/10.1002/ppul.23153
30. Choukroun M, Feghali H, Vautrat S, Marquant F, Nacka F, Leroy V, et al. Pulmonary outcome and its correlates in school-aged children born with a gestational age ≤ 32 weeks. Respir Med. 2013;107(12):1966-76. http://dx.doi.org/10.1016/j.rmed.2013.06.020
31. Vom Hove M, Prenzel F, Uhlig HH, Robel-Tillig E. Pulmonary outcome in former preterm, very low birth weight children with bronchopulmonary dysplasia: a case-control follow-up at school age. J Pediatr. 2014;164(1):40-5.e4. http://dx.doi.org/10.1016/j.jpeds.2013.07.045
32. Zanudin A, Gray PH, Burns Y, Danks M, Watter P, Poulsen L. Perinatal factors in non-disabled ELBW school children and later performance. J Paediatr Child Health. 2013;49(1):E62-7. http://dx.doi.org/10.1111/jpc.12022
33. Jobe AH. An unknown: lung growth and development after very preterm birth. Am J Respir Crit Care Med. 2002;166(12 Pt 1):1529-30. http://dx.doi.org/10.1164/rccm.2209012
34. Kulasekaran K, Gray PH, Masters B. Chronic lung disease of prematurity and respiratory outcome at eight years of age. J Paediatr Child Health. 2007;43(1-2):44-8. http://dx.doi.org/10.1111/j.1440-1754.2007.01001.x
35. Friedrich L, Stein RT, Pitrez PM, Corso AL, Jones MH. Reduced lung function in healthy preterm infants in the first months of life. Am J Respir Crit Care Med. 2006;173(4):442-7. http://dx.doi.org/10.1164/rccm.200503-444OC
36. Friedrich L, Pitrez PM, Stein RT, Goldani M, Tepper R, Jones MH. Growth rate of lung function in healthy preterm infants. Am J Respir Crit Care Med. 2007;176(12):1269-73. http://dx.doi.org/10.1164/rccm.200703-476OC
37. da Silva KS, Nahas MV, Peres KG, Lopes Ada S. Factors associated with physical activity, sedentary behavior, and participation in physical education among high school students in Santa Catarina State, Brazil [Article in Portuguese]. Cad Saude Publica. 2009;25(10):2187-200.
38. Clemm H, Røksund O, Thorsen E, Eide GE, Markestad T, Halvorsen T. Aerobic capacity and exercise performance in young people born extremely preterm. Pediatrics. 2012;129(1):e97-e105. http://dx.doi.org/10.1542/peds.2011-0326
39. Dumith SC, Hallal PC, Menezes AM, Araújo CL. Sedentary behavior in adolescents: the 11-year follow-up of the 1993 Pelotas (Brazil) birth cohort study. Cad Saude Publica. 2010;26(10):1928-36. http://dx.doi.org/10.1590/S0102-311X2010001000009
40. Hamar P, Biddle S, Soós I, Takács B, Huszár A. The prevalence of sedentary behav-iours and physical activity in Hungarian youth. Eur J Public Health. 2010;20(1):85-90. http://dx.doi.org/10.1093/eurpub/ckp100