BACKGROUND The kidneys and lungs share the mutual task of maintaining acid-base homeostasis. Abnormalities in fluid balance, blood electrolytes, hemoglobin concentration (Hb), and vascular tone in chronic kidney disease (CKD) may have profound effects on respiratory function. Chronic lung disease and CKD frequently coexist,(1) creating further challenges to pulmonary function tests (PFTs) interpretation.
OVERVIEW A 68-year-old man under long-term hemodialysis (HD) and progressive exertional dyspnea underwent PFTs as part of the workup pre-kidney transplant. Spirometry suggested, and body plethysmography confirmed, mild restriction. Hb-corrected DLCO and KCO were severely reduced; further workup confirmed mixed pre- and post-capillary pulmonary hypertension (PH). Despite comprehensive treatment, the patient died before transplantation (patient A). A 77-year-old woman with "mild" COPD on spirometry presented with severe hypoxemia (¯ PaO2) but only mild-moderate decrements in SpO2 ~two hours within the HD sessions. Detailed assessment of gas exchange in a subsequent session showed similar decrements in the alveolar pressure for O2 (PAO2) and a measured respiratory exchange ratio (RER; CO2 output/O2 consumption) of only 0.63 (0.85 pre-HD). She was diagnosed with HD-induced hypoxemia (patient B).
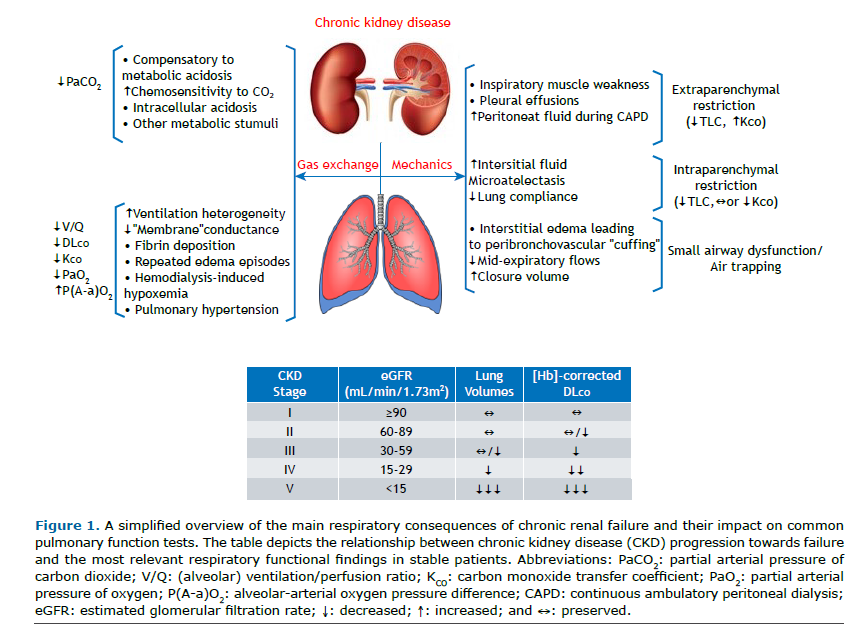
CKD patients often develop a mild restrictive spirometry pattern, which has been traditionally ascribed to chronic fluid overload. They show an exquisite sensitivity to develop "flash" interstitial edema over time, causing repeated episodes of acute-on-chronic restriction. However, lung volumes may decrease without overt edema, likely reflecting interstitial structural abnormalities and low compliance.(2) When the glomerular filtration rate decreases further, pulmonary edema, pleural effusion, and respiratory muscle dysfunction are more common. Electrolyte disturbance may also contribute to skeletal (including respiratory) muscle weakness. In some patients, apparent restriction on spirometry is not due to low TLC but higher residual volume, likely due to early closure of the dependent small airways (Figure 1).(3)
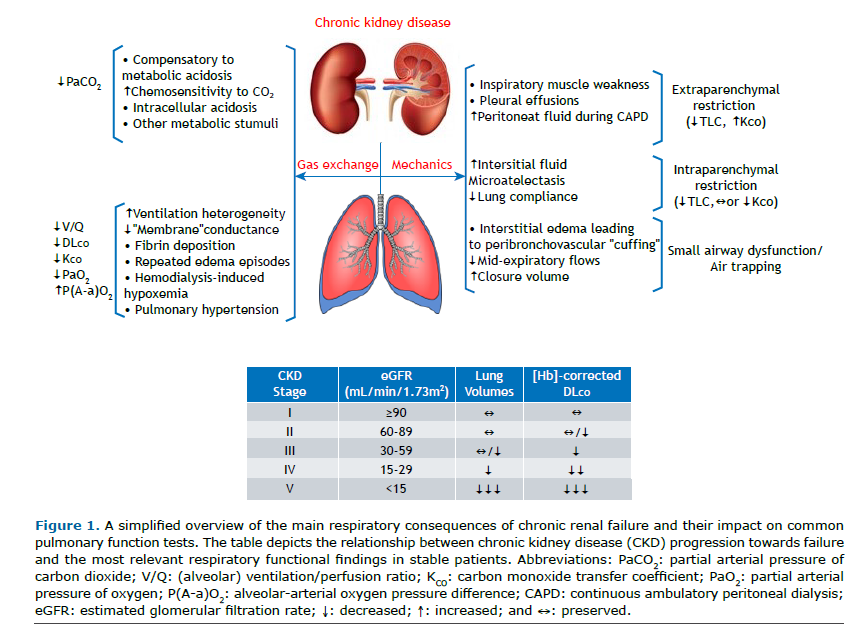
Anemia is a major determinant of low DLCO (and KCO) in CKD. Interestingly, both may remain low after Hb correction. This has been ascribed to lower "membrane" conductance rather than impaired capillary blood flow.(4) It remains present after dialysis and may not completely reverse after kidney transplantation.(2) The underlying mechanisms are unclear, but akin to heart failure, it may result from the deposition of fibrin following repeated episodes of clinical or sub-clinical edema. Low DLCO may also signal PH, a comorbidity closely associated with poor prognosis (patient A).
Some patients-particularly those with underlying lung disease-may develop significant hypoxemia as the HD session progresses. Several mechanisms have been put forward; most evidence points out the loss of CO2 into the dialysis fluid. The non-respiratory loss of CO2 causes a lower CO2 output at the mouth, leading to hypoventilation and a lower RER. Since PAO2 = PiO2 - (PACO2/RER), a low RER implies lower PAO2 and, consequently, lower PaO2.(5) A shift in the O2 dissociation curve due to the increasing pH explains why SpO2 may underestimate the severity of hypoxemia (patient B).
CLINICAL MESSAGE Most centers recommend "full" PFTs pre-kidney transplantation for higher-risk patients, i.e., dialysis for an extended period, diagnosis of COPD, history of tobacco exposure, obstructive sleep apnea, previous pulmonary embolism, and/or suspected PH.(6) Close interaction between nephrologists and pulmonologists is paramount, given the bidirectional nature of the observed abnormalities in a population that may present with preexisting, frequently underrecognized lung dysfunction.
REFERENCES 1. Navaneethan SD, Mandayam S, Arrigain S, Rahman M, Winkelmayer WC, Schold JD. Obstructive and Restrictive Lung Function Measures and CKD: National Health and Nutrition Examination Survey (NHANES) 2007-2012. Am J Kidney Dis. 2016;68(3):414-421. https://doi.org/10.1053/j.ajkd.2016.03.415
2. Sidhu J, Ahuja G, Aulakh B, Narang A, Whig J, Sidhu U. Changes in pulmonary function in patients with chronic renal failure after successful renal transplantation. Scand J Urol Nephrol. 2007;41(2):155-160. https://doi.org/10.1080/00365590600991557
3. Gembillo G, Calimeri S, Tranchida V, Silipigni S, Vella D, Ferrara D, et al. Lung Dysfunction and Chronic Kidney Disease: A Complex Network of Multiple Interactions. J Pers Med. 2023;13(2):286. https://doi.org/10.3390/jpm13020286
4. Moinard J, Guenard H. Membrane diffusion of the lungs in patients with chronic renal failure. Eur Respir J. 1993;6(2):225-230. https://doi.org/10.1183/09031936.93.06020225
5. Patterson RW, Nissenson AR, Miller J, Smith RT, Narins RG, Sullivan SF. Hypoxemia and pulmonary gas exchange during hemodialysis. J Appl Physiol Respir Environ Exerc Physiol. 1981;50(2):259-264. https://doi.org/10.1152/jappl.1981.50.2.259
6. Sahni S, Molmenti E, Bhaskaran MC, Ali N, Basu A, Talwar A. Presurgical pulmonary evaluation in renal transplant patients. N Am J Med Sci. 2014;6(12):605-612. https://doi.org/10.4103/1947-2714.147974


 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Pocket
Pocket